June Aman no longer laughs when her husband teases her, which he does fairly often. When she complains about how long it takes Dave to fix something, he says she never told him she was in a hurry. When she says he has no one else to pick on, he responds, "You poor thing." Sometimes, he speaks about her beauty in the past tense and doesn't correct it when she needles him about it.
She stiffens when the man she has been married to for the past 56 years pokes at her. His stings hurt June, but they also worry her, because she's not sure when he's kidding or when he's covering up his inability to contribute anything else to the conversation. Three years ago, Dave was diagnosed with Alzheimer's disease. And when he jokingly says of the doctors who made the diagnosis, "What do they know?" the knot inside June tightens.
Dave and June were born three days apart and have known each other since they were 10, growing up across the street from each other in the northern reaches of New York state. They dated as teenagers, married at 18 and raised six children. They still hold hands and gaze into each other's eyes, but these days the look in Dave's eyes is cloudy and glazed. He seems absent, and it's hard to tell if he's following a conversation or just pretending to. And June never knows when his teasing is done with endearment or when it's hiding the fact that his mind is eroding.
Soon, Dave will probably forget who June is. Already, he is incontinent, unable to dress himself and occasionally verbally abusive. They had just sold their farm and begun enjoying their retirement when Dave's symptoms began. "I get angry with God," June says.
June and Dave live in the small town of Ontario, New York— just a couple of miles from the shores of Lake Ontario, where they've spent their entire lives. The region was covered in farmland until not too long ago. Rochester, the closest city, is just 25 miles away. But the Amans grew up surrounded by crops and orchards, square dancing with their families for weekend entertainment, and with little access to transportation. Their decades of country living make Rochester seem like another world. June and Dave are rural Americans living in rural America.
For June, living in rural America means endless hours alone with a husband who is increasingly unable to take care of himself. Their rhubarb and curly willow crops are gone. Family members rarely show up unannounced anymore. Their children have moved away. It is enough to make anyone angry with God. For many people, caring for someone with dementia in rural America is a version of hell.
The United States is aging fast. In 2020, the oldest members of the baby boom generation—the nearly 73 million Americans born between 1946 and 1964, of whom about 65 million are still alive—will be 74 years old. Currently, about 75 million Americans are between the ages of 51 and 69. This rapidly expanding elderly population means an accompanying rise in the number of people living with the degenerative brain condition known as dementia. One in 10 Americans age 65 and over—an estimated 5.5 million people—has been diagnosed with Alzheimer's disease, the most common type of dementia. By 2030, more than 8 million Americans will be living with some form of dementia.
Rural America is being hit particularly hard. The migration of young adults fleeing farming communities coupled with the movement of retirees to pastoral settings is tipping rural demographics toward people age 65 and older. A recent report by the U.S. Department of Agriculture predicts a significant swelling of the retirement-age population in rural America, where the death rate is 14 percent higher in the nation's least populated counties than in the most populated ones.
In rural areas, the rising proportion of older Americans means an accompanying rise in people with dementia. And these counties do not have the money, the professionals or the services to address the coming tidal wave of cognitive decline. Distance, poverty and lack of access to health care providers make it increasingly difficult for caregivers to help those with dementia. As a result, they carry a heavier load, with the psychological isolation compounded by a physical one. Unable to cope, family members often move their loved ones to long-term facilities. The cost of formal aid for dementia is estimated at $259 billion per year in the U.S.
But New York has a radical plan to save the caregivers by helping them take a break. Or have a shower. Or run errands. Or maybe just nap. The state has dedicated $62.5 million over five years to support caregivers. And New York is not alone in its epiphany. Such state-funded programs have cropped up across the country, particularly in rural states, such as North Dakota, Minnesota and North Carolina. Together, these initiatives could save billions of dollars. And they could make life bearable again for people like June Aman.

Eating the Brain Slowly
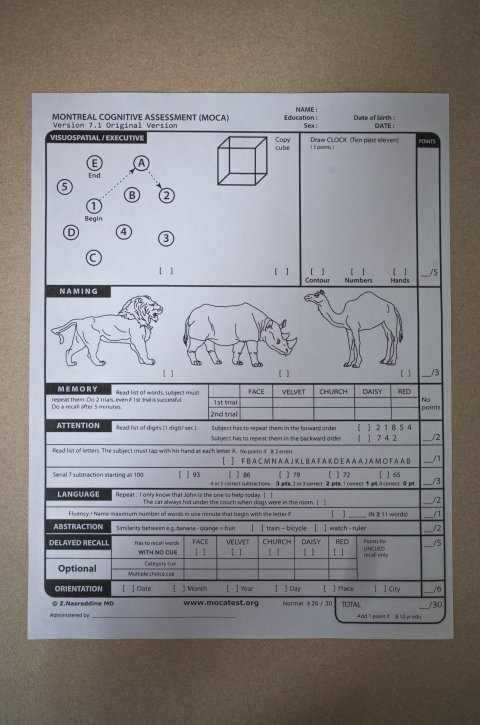
Dementia is broadly defined as cognitive or memory impairment in a person who is still conscious and alert. You can get the attention of someone with dementia, but you can't necessarily hold it for very long. Some people lose their short-term memory. Some hallucinate. Others become ornery or lose their inhibitions in public. Some have all these symptoms and more. Whatever the manifestation, all forms of dementia are united by a single fact: A neurocognitive disease is killing the brain. Alzheimer's and other forms of dementia are the sixth-leading cause of death nationwide.
Alzheimer's is unstoppable. Aside from a few medications that diminish some symptoms for some patients, there are no treatments. Researchers are studying various dietary changes to delay progression of the disease, but none have so far been proved to work. The disease tends to eat away at the brain slowly, so the afflicted person lives with the disease for an average of nine years, sometimes much longer.
Caring for someone with dementia is more than a full-time job; it is a full-life job. People with dementia need help bathing and dressing. They cannot prepare food or feed themselves. They can't manage their medications, and they can't make doctor's appointments or get to them. Sometimes, they cannot even leave their bed or a get up from a chair without assistance. They have a disturbing tendency to wander. "It's a scary illness," says neuropsychologist Richard Durant, clinical director of the Center for Neurobehavioral Health, part of the State University of New York in Plattsburgh. For caregivers, the slow speed at which the disease erodes the brain means years of long days with a spouse or parent who no longer recognizes wives, sons or daughters; of heaving an uncooperative body into the shower; of not knowing what brain-controlled function, such as the ability to swallow, will disappear next.
An estimated 15 million people in the U.S. are informal caregivers for people living with dementia. Mostly wives and daughters, caregivers tend to also handle ancillary tasks, like paying bills or talking with doctors. Americans dedicate about 18.2 billion hours of unofficial assistance to dementia each year, an estimated $400 billion worth of unpaid time.
Despite the magnitude of the job, caregivers often resist seeking professional help until the disease has progressed to an unmanageable state. Valerie Drown, a mental health counselor with the Center for Neurobehavioral Health, tells the story of a caregiver whose husband got in his car to get coffee and ended up in a town two hours away, unaware that he wasn't where he said he'd be. After years of less alarming forgetfulness, this event pushed his wife to call Drown. Caregivers often arrive at Durant's clinic after the person with dementia has started hallucinating or can no longer sustain a conversation. "To us, that's gone too far already," says Durant. By the time they reach out to support services, the caregivers have missed the chance to prepare themselves and are at the bottom of long waiting lists for the help they desperately need.
The challenges of supporting people with dementia are greatly exacerbated in rural areas. Traveling to a doctor—or just the supermarket—can be difficult, especially during rough winter weather. Health care is not always within reach: Although 20 percent of Americans live in the countryside, only 10 percent of doctors practice there. Across the U.S., people willing to work in elderly care are in short supply, and the scarcity is worse in rural areas.
Family dynamics often become fraught. Children who have migrated to urban communities cannot help the caregiving parent. Those who've remained "feel that all this fell on their shoulders," says Brad Gibbens, deputy director of the Center for Rural Health at the University of North Dakota School of Medicine and Health Sciences. And the caregivers, who are mostly in their 60s and coping with their own ailments, feel abandoned and isolated. "Where are the kids? Why aren't they here?" says June. "I don't feel terribly supported by them."
Dementia takes a bitter toll on caregivers. Up to 40 percent of these individuals suffer depression, far higher than the general population in the same age group. They are more likely than their peers to be financially strapped. They are also more likely to begin their own cognitive decline. "These cumulative stresses on caregivers dull their senses, their affect and everything about their function," says Carol Podgorski, who directs the Memory Care Program at the University of Rochester Medical Center. "I forget things," says June. "I get worried about me."

Keep Them Home
In the early 1980s, dementia slowly pulled Mary Mittelman's mother away from her. That trauma led Mittelman, an epidemiologist at New York University School of Medicine, to wonder how she and her brother could have coped better. "I felt that our family could have used some kind of support, though I had no idea what." She decided to turn a family drama into scientific inquiry. That pursuit would become the focus of her career—and bring desperately needed attention to the plight of dementia caregivers.
Mittelman wanted to know whether providing more and varied types of counseling to caregivers would benefit them and the dementia sufferers. She designed a randomized clinical trial to compare outcomes among families who received extra opportunities for counseling versus those who did not. The study, which began in 1987, lasted 18 years and included 406 spouses of people with dementia. The control group had access to basic support—brochures and a phone number for expert help—and the experimental group received two individual counseling sessions and four family counseling sessions in four months, access to telephone counseling when they needed it and encouragement to join a weekly support group.
The results confirmed Mittelman's hunch that when it comes to caregiver support, more is more. Families that received the experimental approach placed their loved one in full-time facilities an average of a year and a half later than the control families. The prolonged time at home was attributed to two benefits of the extra help: Caregivers were better able to respond to behavioral problems rooted in dementia, and they were less depressed.
Keeping people with dementia at home longer can help slow its ravages. As the disease progresses, sufferers become less able to adapt to new surroundings. The unfamiliar setting of a nursing home or assisted-living facility—even a seemingly innocuous change, like which side of the bed they must get out of—may cause stress and speed up cognitive decline. "Absolutely everything is new to that patient," says Gibbens, "and they get confused."
Aging in place, as clinicians refer to living where one chooses, also saves money. In Washington state, which has the highest rate of Alzheimer's disease in the country, nursing homes cost an average of $97,000 per year. At $55,000 per year, assisted-living facilities are better but hardly affordable to all but the wealthiest. Every year, Medicare spends an estimated $22,000 per person on nursing homes and skilled nursing facilities for beneficiaries with dementia, compared with about $1,100 on the same expenses for people without dementia. A 2014 study by Mittelman and several Minnesota-based health economists and epidemiologists concluded that her caregiver intervention program could save the state up to $996 million between 2010 and 2025. In North Dakota, where a third of the state's population is rural, the potential cost savings from a caregiver program was estimated at over $12 million a year.
But for Mittelman, caregiver intervention is not about the bottom line. "Our primary goal was to improve the well-being of the family member. If the caregiver can't cope, it's a much more difficult and less satisfactory outcome for the person living with dementia." To help the patient, rescue the caregiver.
'You Want to Remember'
About 10 years ago, Andrew Straight found his grandmother, Annie, standing in the middle of the road. "She didn't know where she was," he says. Annie was diagnosed with Alzheimer's disease in 2009. Now, she spends her days in a recliner, next to one still molded to the shape of her husband, who died two years ago. She cannot carry on a conversation. She recalls almost nothing about her life: not the rock she used to stand on while she sang to the sky as a little girl, not her close-up encounter with a bear on the mountain by her home in New York near Lake Placid, not winning a midget race car competition. She remembers her losses—the son who died in his 30s in a car accident, her husband—but not always clearly or correctly. "It's gone by so fast. You want to remember because you know it's important," says Annie, 83. "I can't remember."
She can respond to a question posed to her but cannot follow a conversation. "I never know whether things are right, or exactly right, or if people just made them up as they went along, or if people were making them up hoping they happened," she says in a rare moment of lucidity.
Annie needs constant care. She sleeps in a hospital bed with the side rails up to deter her from getting up at night. Her primary caregivers—her son, Jeff, and his wife, Sharon—keep a video baby monitor in her room so they can check on her at night. Although she mostly watches television or looks out the window from her recliner during the day, Annie cannot be left alone. "She's a two-person assist," says Jeff.
After Annie's husband died, Jeff and Sharon, who were living two hours away, moved back to Jeff's childhood home, a farmhouse north of Lake Placid built by his ancestors in 1841. Andrew, who is 42, and his children also moved home, making it a four-generation household. They all take care of Annie because Jeff and Sharon are determined to keep her out of a nursing home. "As good the care is that they could give her," he says, "they can't give her the care we can here." Andrew's children willingly help. Troy, 17, likes to sneak her candy. Mackenzie, 20, who recently moved two hours away, spends one week of every month at home. Hayley, 15, says her friends are impressed by their dedication. "It's really cool that you guys are like an actual family," they tell her.
But all that help is still not enough. Until a few months ago, Sharon, 62, had not been to a doctor in two years. Jeff, 64, has metastatic prostate cancer that will soon require hormone treatment. They have both neglected the physical therapy their doctors recommended because of lack of time. Andrew installed a rudimentary gym in the basement, but they can't leave Annie's side for long enough to go downstairs for an hour.

Finding help is hard. The closest neurologist specializing in dementia is in Albany, more than two hours away. Their doctors are in Plattsburgh, an hour away. Their town has 2,500 people—few, if any, of whom are home health aides. Because Jeff and Sharon lived a couple of hours away before moving home to take care of Annie, they have few connections in the area. "I don't have anybody," says Sharon.
They sought assistance through Alzheimer's support programs, but their rural location was always an obstacle. "That's why we're using the family," says Jeff. "It's hard to find other folks that are willing."
'No Room for Anything Else in His Head'
The emotional and financial anguish of the dementia epidemic is pushing states to find new and viable solutions. New York has taken an unexpected approach: providing an unprecedentedly large amount of money to support caregivers. In late 2015, New York Governor Andrew Cuomo announced a $67.5 million grant to help the estimated 1 million people providing informal dementia care in the state. Nine organizations are receiving $7.5 million over five years to provide assistance that people like the Straights and the Amans have been missing. Cuomo also designated an additional annual $2.3 million for five years to 10 Centers of Excellence for Alzheimer's Disease for on-site clinical support of patients and their caregivers. The amount puts dementia caregiving on par with services to help prevent cancer and chronic diseases like diabetes and asthma. "New York went from a state that had some support to the state that has the most support," says Podgorski, whose facility received a Center of Excellence grant. "It's been huge."
The funding program, called the Alzheimer's Caregiver Support Initiative, is modeled on Mittelman's caregiver intervention. The $7.5 million per year, administered by the Department of Health, pays for private and family counseling, a 24-hour help hotline, support groups, local education sessions and "joint enrichment" activities that dementia sufferers and their caregivers can do together. Separate from Medicare, Medicaid and federal health insurance law, the funding is unusually free from red tape. The money also covers emergency response for wandering. "It's our responsibility to be there," says New York state Commissioner of Health Howard Zucker, "to assist in easing any of the burdens that caregivers face."
But by far the most popular part of the grant is the respite hours. Caregivers can use the money to hire neighbors, friends or other non-professionals to stay with their loved one for $15 per hour, with no financial eligibility requirements attached. "It's open to caregivers who need it," says Yvonne Lott, who manages the grant money awarded to the Center for Neurobehavioral Health at the State University of New York, Plattsburgh. That means people who don't qualify for Medicaid but who cannot afford private care on their own can now obtain assistance. "Those are the people I worry about," says Drown, of the Center for Neurobehavioral Health.
New York is not the only state to offer direct support to caregivers. North Carolina, which is 80 percent rural, has had caregiver support funding since 2001, although the respite hours were eliminated due to budget cuts in 2011. North Dakota has a similar program operated in partnership with Minnesota. But the quantity of funding provided by New York to caregiver support is many times larger than any prior attempt. "The impact has been immediate," says Teresa Galbier, head of the Rochester and Finger Lakes Region Alzheimer's Association.
Jeff and Sharon were among the first people to receive respite hours through SUNY Plattsburgh. They each have up to 120 hours per year to spend on other informal caregivers. They've used the time for appointments with their own doctors, tending to household chores and going away together. Jeff credits the program with enabling them to continue caring for his mother. "It's the reason we can keep her home," he says.
The initiative also pays professionals to travel to families instead of the other way around. Some caregivers hate speaking about dementia in front of the spouse or parent who has it, but they can't leave that loved one at home while they travel to a clinic. Others can't drive long distances. The grant pays counselors like Drown to travel far and wide to meet caregivers, which facilitates private conversations in familiar settings and reduces stress. "Our job is to meet them wherever they're most comfortable," she says.
All of these new options are bringing profound relief to caregivers, particularly in rural areas, and saving huge amounts of money. Typical out-of-pocket costs for dementia support can exceed $80,000 for the duration of the disease, with much of that spent on home health aides. But it turns out that the healing provided by the funding is reaching even deeper, offering an escape from lifelong wounds brought to the surface by the stress of Alzheimer's caregiving.
June Aman had long battled a negative self image, first as a child growing up with a mother who called her dumb and ugly, later as a florist who closed her business after a mental breakdown—"I couldn't handle things very well," she says—and as the wife of a crop-obsessed farmer. "There wasn't room for anything else in his head," she says, "meaning me."
That history has made it hard for June to handle the meanness that has bubbled up in Dave as part of his dementia. "I have a very bad self-image," she says, "and Dave hits right to the core."
Yet their love, which has been part of nearly their entire lives, continues to fuel June's fierce protection of her husband, who denies he has Alzheimer's disease. "My memory has a hole in it," he admits, but that's as far as he will go. He disagrees with the diagnosis made by his neurologist at the University of Rochester Medical Center. Such denial is common and prevents caregivers from speaking openly about their situation. But when someone doesn't acknowledge dementia, says Mittelman, then the caregiver cannot be recognized as such and can't get help. "Then you become isolated," she says. Like many caregivers, June worries about wounding her husband's dignity and pride, which keeps her from sharing his diagnosis, which in turn makes life harder for her. "It makes June carry a large secret," says Podgorski, "which also contributes to her isolation."
The Alzheimer's Caregiver Support Initiative pays for counseling sessions with Podgorski, which June says have helped her enormously. "She has a sanctuary where she can say things out loud," says Podgorski. Having someone to talk to has transformed June. "I have more strength than I thought I had," she says. She finally told her family that she and Dave need them to visit more, and she mustered the courage to share her story here. And she has learned to not take Dave's darker moods personally. "I just get up and leave," she says. Now, when they stand outside for a photograph, their demolished barn in the background and the ground at their feet strewn with twigs of curly willow, the love that has carried them through 56 years visibly outshines the wounds and discomforts.
Drown says the money provides more time for what caregivers often need most: to talk. She receives regular phone calls from caregivers at their wit's end, "crying because someone is taking the time to just listen," she says. And the duration of her counseling sessions is unlimited.
The program also helps caregivers navigate an increasingly confusing health care system. An upcoming shoulder replacement surgery will make it impossible for her to take care of Dave for weeks or months. A social worker, paid by the initiative, identified assistance she is eligible for through insurance and other federal- and state-funded programs, something she could not have done on her own.
The initiative doesn't solve all the problems facing dementia caregivers. A 2008 report by the Institute of Medicine laid bare the extreme shortage of geriatric professionals, including doctors, nurses, psychiatrists and social workers. Little has changed since this forewarning, and the new program does not alter the paucity of the workforce. Salaries are such that a fast-food restaurant employee may earn the same as a home health aide, providing little financial incentive to pursue the latter, more rigorous work.
The uncertainty of health care coverage at the federal level means families like the Amans and the Straights cannot count on affording their own care. Medicare now reimburses providers for time spent with patients discussing strategies to prevent illness and covers cognitive screening, which could lead to more earlier diagnoses of dementia. But how changes to federal health care law will affect older Americans remains unknown, especially in light of the uncertain future of the Affordable Care Act.
And no matter how much help is provided, there is no guarantee that a caregiver will seek it out. Older members of the baby boom generation typically resist becoming a burden upon others, says Zucker. "That generation, as a group, is much more independent," he says. Among rural Americans, that independence streak runs particularly thick. "They kind of suck it up and deal with it as a family," says Gibbens, who grew up on a farm in North Dakota. "We do not take pity," says Sharon, who has arthritis and fibromyalgia, of the Straight family caring for Annie. "Pain is your friend. When you die, you'll be out of pain."
Still, programs like New York's initiative are a huge step toward a sustainable response to the dementia epidemic. They are also inspiring a new generation to rethink their attitude toward the elderly. "I want to be the person to volunteer," says Annie's great-granddaughter, Mackenzie, who is planning to become a certified nurse assistant. "I would love to help out a family so they can have a rest, because we know how exhausting it can be."