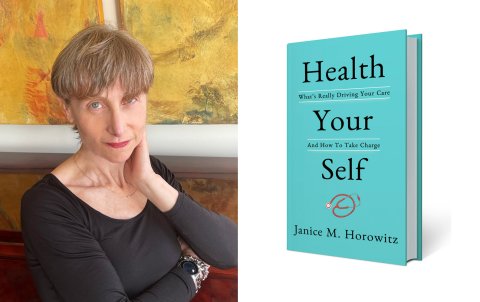
When you're sick and deciding whether to go to the doctor, there are many factors to consider, especially with the Delta variant lingering and multiplying. Should you go to urgent care? Wait to see your primary care doctor? Is telehealth better than an in-person visit? How do you decide? Newsweek talks with veteran former Time health reporter and host of public radio's Dueling Docs: The Cure to Contradictory Medicine, Janice M. Horowitz about these issues and other ways to take charge of your health in this Q&A. And find out more about the background forces that can compromise care in her new book, Health Your Self(Post Hill Press, September 21).
Urgent care centers are so convenient. Should the default be to go to your family physician instead? Even if it means waiting days (or longer) for an appointment?
If your symptoms suggest COVID, don't wait. Call your doctor, sure, but hightail it to a testing site for a nasal swab. Unfortunately, just about any symptom is suspect these days, including fatigue, vomiting and even sniffles.
Urgent care trumps waiting for your family physician for splinters, minor burns, bug bites, suspicions of a bone break and even minor chest pain. But your family doctor knows you, so is always a better choice generally, and anytime something she's following flares up. Don't be shy about asking to be squeezed in.
When you do go to urgent care, how can you ensure continuity of care? What do you need to do afterward to keep your physician in the loop?
Urgent care should send a report to your doctor and will tell you how to follow up. Many people ignore the advice. Understandable for problems that go away, such as an earache. But for anything more serious, be a good patient and get to—or at least talk to—your family physician.
What are your best suggestions for how to be assertive with medical professionals without rubbing them the wrong way?
Always be polite. Doctors are people, too, and they respond better to patients they get along with. And never hint that you are the type who might sue. Ask sincere questions to open a discussion so your doctor feels interested in your case. That will free her up to think broadly about you as an individual, instead of just following the strict guidelines issued by medical societies. You are, after all, your own person, with your own immune system, lifestyle and all the imponderables that make you, you.
Do you suggest the same kind of approach with all types of medical professionals? Would you handle your private physician or nurse practitioner differently than an urgent care doctor?
With all your providers, I want you to be a skeptic—but not a cynic. For example, if anyone suggests a drug you need for life, a red flag should go up. Daily medications are more likely to have long-term side effects. Before diving in, ask to repeat the blood test that might have triggered the "lifer" prescription initially. Private physicians and nurse practitioners can monitor you and follow up, neither of which is the role of an urgent care or E.R. doctor who sees you once, and then moves on.
You've discussed cases where doctors are influenced to overtreat. But what about where you fear your concerns are not taken seriously?
This goes back to one of the most essential components of good health care: time. If you think your doctor is dismissive, ask to schedule another visit to continue the discussion.
Keep a file of all your X-rays, MRIs and other reports. If you come armed with objective evidence of a problem, you're sure to be taken more seriously.
COVID-19 has turned everything on its head. Nonessential surgeries were canceled, and people skipped preventative care appointments to avoid contact with sick people. Is now the time to schedule all those in-person checkups?
Absolutely yes. But there are COVID surges throughout the country, so do it right: Get the jab in your arm and mask up before you go.
See a physician now for suspicious moles and severe back pain and headaches, among countless other potentially serious concerns. Don't put off screening tests either, such as a colonoscopy or mammogram. And do not ignore what's shaping up to be an epidemic inside an epidemic: struggles with mental health.
During the pandemic, many appointments were converted to televisits. What types of appointments should you do in person, if possible? What about telehealth?
Telemedicine is best suited when your symptoms are easy to talk about, and if necessary, visible. Good candidates include: arthritis, colds and flu; skin rashes; diarrhea; and therapy. You want actual facetime for anything medically complicated, such as unexplained fatigue, chronic chest and abdominal pain—and obviously for broken bones, X-rays and dental work. Kids almost always do better face-to-face. Remember: you can always start with telemedicine and then switch to in-person.
What resources do you recommend for reliable health information?
Try government sites first. The information is vetted, carefully curated and written in understandable language. They include the Centers for Disease Control, the National Institutes of Health and the Food and Drug Administration. Also check out sites associated with medical centers such as the Mayo Clinic and the Cleveland Clinic.