As the world grapples with the reality of living with COVID-19, a rogue's gallery of deadly pathogens seems to have stepped up the attack. Monkeypox, a close relation of smallpox, is officially a public health emergency worldwide. The current outbreak—the first large one ever outside of Africa—has spread globally to more than 45,000 people, including more than 16,000 confirmed cases in the U.S. And polio, a disease routinely referred to as "eradicated," is circulating in and around New York City and London, bringing with it the irreversible paralysis that strikes about one of 200 people infected with the disease.
These two headline-grabbing afflictions are only the most visible elements in a spate of new outbreaks. The world seems to be entering a new, deadly era of health threats from infectious diseases—old ones we thought we'd wiped out, and new ones on the rise. "It feels like COVID-19 has opened up a Pandora's box of infectious disease surprises," says Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota. "What's next?"
Why this deadly trend is happening at this particular moment is something of a mystery. The rise in anti-vax sentiment and the politicization of public health during the pandemic hasn't helped, but a panoply of other factors seems to be in play, too—including, in the case of polio, vaccines themselves. In recent years, commercial development has brought more people into contact with new diseases. Climate change has helped diseases spread to new animal and human populations. Airplane travel means an outbreak in one part of the world can quickly spread to another. And better testing is revealing outbreaks and new pathogens that might previously have gone unnoticed (the optimist's view).
Whatever the cause, now would be a particularly bad time for a new pathogenic threat. Ironically, the world may be less prepared than before the pandemic. The stunning failures of various global and national public health systems in the face of COVID-19 have yet to be fixed. China, which kept quiet about the initial outbreak when it might have been contained, is if anything more tight-lipped now. The World Health Organization (WHO), which proved unable to slow the disease's rapid spread to the rest of the world, has yet to address its shortcomings. And the U.S. Centers for Disease Control and Prevention (CDC) today faces a massive reckoning over its own poor performance. Vaccination rates have slipped, and the general public today has less patience for public health measures aimed at containing the spread of disease than it did two years ago.
When it comes to technology, things look better. During the pandemic, the biotechnology industry had a chance to flex its muscles in whipping up vaccines and treatments custom-made to fight specific viruses. Those same tools—and new ones coming online almost daily—will be at hand to at least help mitigate the damage from whatever the next fast-spreading infectious disease has in store for us. Whether it will be enough to keep most of us safe is an open question.

Old Threats Redux
Infectious outbreaks and epidemics have a long history of mowing down wide swaths of the population. In 170 A.D., a plague (probably smallpox) killed 5 million Romans, bringing the empire to its knees. The Black Death (bubonic plague) may have killed 200 million Europeans in 1346. Explorers to the Americas brought diseases that wiped out about 90 percent of the indigenous population. By some estimates, the Spanish Flu of 1918 killed 50 million people.
Since then, infectious diseases seemed to recede into the background, thanks to modern medicine and its vaccines, antibiotics and other tools. "For 99 percent of human history, the microbial world killed us at will," says Amesh Adalja, senior scholar at the Johns Hopkins Center for Health Security. "Then, for the last several decades, we had the science and technology to beat back the hordes of pathogens."
Or so it seemed, until COVID-19. And now, while we're still reeling from the latest variant-driven surge, two diseases most of us thought were in our rearview mirror—smallpox and polio—have had a resurgence.
Smallpox used to kill a third of its victims. It was declared to be eradicated in 1980, but monkeypox, a close cousin, has a fatality rate of 5 percent, more or less, depending on the strain. Having jumped to humans from monkeys by 1970, monkeypox has since infected hundreds of people mostly in Central and West Africa. The current outbreak—the first large one ever outside of Africa—started in May in the U.K., apparently through someone who had traveled to Nigeria.
Although the virus has circulated mainly among men who have recently had sex with other men, it has already begun to spread beyond that demographic. Fortunately, the disease responds well to antiviral drugs, especially Tecovirimat, or TPOXX. CDC researchers confirmed in August that the monkeypox virus can linger for hours on household items. In August, researchers in the U.K. reported that a man who hadn't had sex in months apparently contracted the disease at an outdoor concert, and New York State reported its first pediatric case of the illness.
"We're already seeing other mechanisms of transmission," says Osterholm. "There have been several infections in kids, through household contact with clothing or bedding, and we'll start seeing more cases in women who are partners of bisexual men."
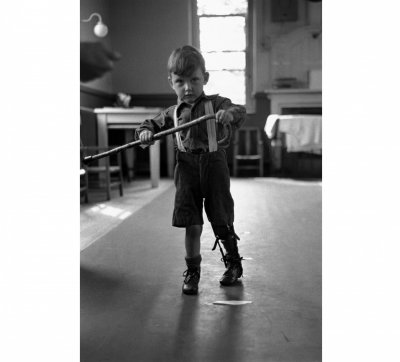
The reemergence of polio as a threat is even more jarring. The disease terrified Americans through much of the first half of the 20th century, paralyzing more than 15,000 people in the U.S. per year. The availability of a vaccine in the 1950s essentially stamped it out, with the last U.S. case of "wild" polio—that is, polio as it has normally spread for thousands of years—occurring in 1979. The vaccine all but eradicated it globally as well, with a mere six cases popping up in 2021, and only in Afghanistan and Pakistan.
Now, new infections are arising from the vaccine itself—in particular, from the oral version. Unlike the shots given in the U.S. and most industrialized countries, the oral vaccine relies on a live, albeit weakened, sample of the virus. That virus has apparently mutated into forms that can cause illness and spread through feces, causing about 1,000 cases a year, almost all in poorer countries that rely on the oral vaccine.
Travel has brought the odd case of polio to the U.S. over the years, but now it is spreading through "community transmission." In June, paralysis struck an infected man living in New York City's Rockland County suburbs who reportedly had traveled to Poland and Hungary this year. Wastewater testing revealed that the virus is circulating not only in Rockland County, but also New York City. London testing found the virus there, too. Past experience with the disease suggests that for every case of infection that's identified, hundreds of others haven't been picked up because of milder symptoms.



An Expanding Cast
Other, more exotic infectious killers lurking in the background are now coming to the fore. In June, two people in Ghana died from Marburg virus disease. Like Ebola, Marburg causes uncontrolled bleeding, proving gruesomely fatal to anywhere from a quarter to more than three-quarters of its victims, and is untreatable. Transmitted through direct contact with a victim's secretions, Marburg caused outbreaks infecting hundreds in Africa in the 1990s and 2000s, leaving public health experts concerned these new occurrences could presage a spread. "I'm really worried about this one," says Caitlin Rivers, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health. "The hazard is that you don't go hard enough on an outbreak in the early days when it's small, before it's clear what the scale of it might be."
Hepatitis is familiar enough, but it has suddenly begun attacking children under mysterious circumstances. As of the last public report from the WHO on July 8, more than 1,000 children in 35 countries had contracted the illness, and 22 of them had died. Although public data on U.S. pediatric cases is scarce, the CDC confirmed 109 cases in May, noting that 90 percent of the stricken children required hospitalization, a seventh of them needed liver transplants and five of them died. It remains unclear whether some new mechanism—possibly an interaction with a particular cold virus that turned up in many of the cases—is behind the spate of cases.
And in early August scientists revealed in the New England Journal of Medicine that 35 cases of a previously unknown virus, the Langya henipavirus, turned up in patients in two provinces in China. None have died, but viruses related to Langya have in the past caused death rates in as many as three out of four victims. Given the way COVID-19 sprung out of nowhere to rampage globally, any new human viral infection commands close scrutiny and concern. "We just have no way of knowing how a new virus like this will act, or whether it will become rampant," says Katherine Baumgarten, medical director of infection control and prevention at Ochsner Health System in New Orleans.
Bacterial infection remains a threat as well. Tuberculosis still kills over a million people a year globally, and death rates have been rising in recent years—partly because attention to the disease weakened during the pandemic, but also because more virulent, drug-resistant strains are spreading. Case rates remain relatively low in the U.S. The CDC registered a little more than 500 deaths from the disease in 2019. But increasing cases of the most drug-resistant form of the disease is raising concerns of a wider outbreak that might be hard to control.
Lyme disease, a bacterial infection carried to humans by ticks, is on the rise as well, inflicting victims with symptoms that can include everything from cognitive impairment to heart inflammation. In June researchers who had looked at 81 studies of the disease published findings in BMJ Global Health, found that about 15 percent of all humans have had the infection. The CDC calculates that cases have increased by 44 percent over the past 20 years. Meanwhile, the CDC in July issued an alert about Burkholderia pseudomallei, the bacterium behind the disease melioidosis, which kills as many as half the people infected with it. The bacterium had never been found in the U.S., but two cases of melioidosis have turned up in the same part of the Gulf Coast, the second in May. Now the CDC warns the bacterium is likely endemic along much of the Coast.
On the plus side, the U.S. hasn't been hit by bubonic plague—yet. WHO reports a few thousand cases each year globally, usually including a handful of cases in the Southwestern U.S. A more widespread outbreak isn't likely, but neither is it impossible. Weill Cornell researchers found plague bacteria in the New York City subway when they took random bacterial samples in 2017.



Why Now?
Experts aren't certain what—if anything—may be going on to account for the seeming surge of infections across a range of infectious diseases. "It's hard to say whether something different is happening, or whether we're just better able to detect new outbreaks and communicate more about them," says Ochsner's Baumgarten.
If we are indeed becoming more vulnerable to infection, there may be several reasons. For one, anti-vaxxers and many others have let up on getting themselves and their children the vaccines that have long been a routine element of health care. For instance, nearly all adults raised in the U.S. are vaccinated against polio, but vaccination rates have been falling for children in many communities, especially during the pandemic. New York State public health authorities estimate 40 percent of Rockland County's 2-year-olds haven't received the recommended minimum three-dose course of injected polio vaccine.
Part of the reason for the falling vaccination rates may be the toll that the pandemic has taken on people's willingness to get out to the doctor's office. That drop is reflected in the national average vaccination rate for a complete series of standard pediatric vaccinations by age 2, which has fallen to 75 percent from a pre-pandemic rate of about 80 percent. The lower pediatric vaccination rates in many red states suggests that skepticism about public health from conservatives, which has soared during the pandemic, has had an effect. In Louisiana, the pediatric vaccination rate is 62 percent, and in Alaska it has dipped below 60 percent. (Vaccine skepticism has run high in ultra-Orthodox Jewish communities in Rockland County, which was was at the center of a measles outbreak in 2018 and 2019.)
Climate change appears to be playing a role, too. As insects, aquatic life, birds and small mammals are pushed by extreme weather into new territories, they may acquire new infections that they have little protection against, or can pass the infections they've carried from elsewhere on to local animal populations. Viruses in these animals may mutate into forms that can infect humans. With real estate development constantly encroaching on wildlife habitats and bringing humans into contact with animals, these "zoonotic" jumps of viruses from animal to human are becoming more and more likely. A team of University of Hawaii researchers calculated that 58 percent of all known human infections are becoming more dangerous due to climate change. They published their study in Nature Climate Change in August.
Growing exposure to ticks alone is becoming a major source of infection. Nearly half a million new cases of Lyme disease are now turning up each year, and that's only one of a half-dozen serious infections that ticks can pass to humans. Birds, too, are becoming pools of potential zoonotic infections; one strain of bird flu alone has spread through 100 different bird species. Although human infection from birds has so far been rare and well contained, the potential for more serious outbreaks is climbing.
An immediate concern is that animals could play a role in the emergence of new COVID-19 variants. Scientists have already found evidence that the virus has jumped from humans to deer, dogs and cats. It's perfectly plausible that a mutated version could then jump back to humans. Two men living together in France have apparently passed monkeypox on to their dog, reported the medical journal The Lancet in August. "Our single biggest threat is that disease will spill over from the animal world to humans," says Osterholm.
Finally, cities are growing more dense, and travel between nations is on the rise. Even a small, isolated outbreak of a new, dangerous infection—or the reemergence of an old, seemingly defeated one—can now turn into a global crisis in a matter of weeks. Only 12 days after the WHO first called attention to 59 cases of an unusual flu infection in Wuhan, China, the first COVID-19 cases were turning up in the U.S. "In an age of megacities, and travel at the speed of jet," says Adalja, "we're making a trade-off between our ability to socially interact and our ability to contain the spread of disease."


Fighting Back
While the COVID-19 pandemic hit home how vulnerable we are to new infectious diseases, it also highlighted how much better equipped we are than in prior decades to fight these threats through biotechnology. The speed with which scientists genetically and functionally analyzed the virus and used that data to whip up vaccines was unprecedented. It bodes well for our chances of limiting future outbreaks. So does the development of accurate, fast tests, and effective treatments. Advances in these tools and techniques are arriving almost daily, and likely will leave us with even better weapons against the next infectious threat.
We may have another set of weapons at our disposal—many of which were developed decades ago. A growing number of researchers suspect that some or all of the classic pediatric vaccines that have long been given to children prevent polio, measles and other diseases may also work well as adult vaccines against a range of diseases—even against new ones. That's because these vaccines appear to bolster the immune system in a broad way. "We may be able to offer some protection for all people against all emerging pathogens," says Jaykumar Menon, chair of the Open Source Pharma Foundation, which is helping to lead the charge for repurposing these older vaccines. "It's a different paradigm for vaccine science."
It almost sounds like wishful thinking, but there's plausible theory behind it. The new generation of "mRNA" vaccine technologies that were used against COVID-19 focus on helping the body produce antibodies designed to home in on specific molecular targets on the virus. But antibodies aren't the only way that our immune systems fight infection. The so-called "innate" immune response includes proteins, enzymes, acids and other substances that our bodies can produce to block, isolate and attack viruses and other pathogens.
The major childhood vaccines, devised with older methods, also produce antibodies against specific pathogens. But unlike the mRNA vaccines, which focus precisely on specific molecular targets on the virus, the childhood vaccines consist of weakened versions of the actual viruses, which provokes a wider immune response that goes beyond antibodies to boost innate immunity. Evidence suggests they may do so broadly enough to help fight COVID-19 and other novel infections. In a study published in August in Cell Medicine Reports, researchers at Massachusetts General Hospital found that patients with Type 1 diabetes were less than a tenth as likely to get COVID-19 after being given a booster shot of the "BCG" vaccine—a century-old vaccine now routinely given to children to prevent tuberculosis. Other trials against COVID-19 and other respiratory infections are ongoing, and Menon claims preliminary results are encouraging.
Even as science churns out impressive new anti-infection tools, or repurposes old ones, the public health systems essential to effectively deploying the results to the population are proving inadequate. The CDC, the heart of the U.S.' public health system, has been among the list of players roundly criticized for a slow, inconsistent and largely ineffective response to the COVID-19 crisis. The agency's latest, loudest and perhaps most damning critic is the agency's director, Rochelle P. Walensky. Last month, she allowed the public release of a scorching assessment of the agency's performance, based on independent evaluations, along with a call for a major reorganization. "For 75 years, CDC and public health have been preparing for COVID-19, and in our big moment, our performance did not reliably meet expectations," she said in a statement.
Whether a reorganization or any other measure the CDC takes will make a big difference in public health's ability to effectively fight infectious outbreaks is an open question. One big challenge is the uncertain and inefficient way responsibilities are divided between federal, state and local governments.
The CDC can guide, recommend and provide resources, but most of the responsibility for the policies and mechanisms that actually regulate critical behaviors such as quarantines, testing and masking, and that deliver resources such as tests, vaccines and treatments, are controlled at state and local levels. The resulting patchwork of often uncoordinated and even conflicting public health efforts leaves the population vulnerable even when effective tools for fighting an outbreak are at hand. "We're suffering from decades of underfunding at the state level," says epidemiologist Rivers. "We shouldn't be treating a strong public health system as something that's nice to have. It's central to our national security."
Little has been done so far to repair the problem. President Joe Biden's proposed 2023 budget includes $110 billion toward boosting public health's pandemic preparedness, including a $2 billion increase to the CDC's annual funding. But previously proposed funding increases in public health-related spending have struggled to get through the Senate, and it isn't clear yet how much of Biden's proposed funding will survive.
Meanwhile, the CDC and other public health players are already under fire for a slow, muted response to the monkeypox outbreak. "We came into the monkeypox epidemic with all the tools we needed to contain it," says Rivers. "There was no reason it had to circulate here, but now we're no longer in a position of strength to deal with it."
Part of the reason public health experts have been slow to fully confront the monkeypox challenge is that many have hesitated to openly target outreach and resources to the people who are at highest risk—men who have sex with other men—because of the risk of stigmatizing a segment of the population that is vulnerable to unfair treatment. Public health has been slow on the draw in other ways: It took nearly four months for the U.S. to widely deploy tests to communities that most needed them. In spite of a long-standing awareness of a need to stockpile monkeypox vaccines, bureaucratic glitches are still causing a severe shortage of doses. The slow response is on track to become "one of the worst public health failures in modern times," wrote former FDA Commissioner Scott Gottlieb in The New York Times in July.
Slow, inadequate responses to infectious outbreaks is one of America's oldest traditions. During the Revolutionary War, the American army was at the very brink of defeat—not so much due to Britain's superior military, but because, unlike the British, most Americans failed to avail themselves of the readily available innoculation against the raging outbreak of smallpox that was decimating the army. That failure might well have done the American rebellion in, if George Washington hadn't taken control of the situation by ordering mass inoculations, without exceptions, ensuring the remaining troops were able to fight on.
The best weapons are useless if the soldiers won't take up arms. Amid an outbreak, history is a small comfort, especially when it repeats itself.








