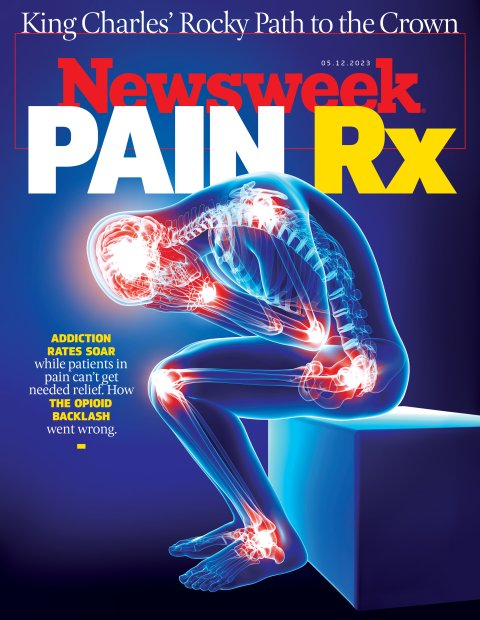
Danny Barcelona lives in constant fear that doctors will stop the medications he considers lifesaving. The 66-year-old has suffered for more than two decades with a debilitating nervous-system disorder and severe back and shoulder pain, forcing him to close his once-thriving dental-lab business in Asheville, North Carolina, and sometimes leaving him bedridden for 18 hours a day. That he can function at all, he says, is due to his ongoing prescription for oxycodone, an opioid.
In the middle of an epidemic of opioid overdoses, doctors, hospitals and pharmacies across America are facing intense pressure to sharply cut back on prescribing and dispensing the drugs. About 8 million patients in the U.S. who depend on opioids to face constant, intense pain are at risk of losing access to the one treatment that seems to make the pain bearable. That includes Barcelona. "I don't think I could have lived without the drugs I've been taking," he says.
The number of opioid prescriptions has plummeted from a high of 251 million in 2010 to well under half that number in 2020—the last year for which figures are available from the U.S. Centers for Disease Control and Prevention (CDC). Yet the number of opioid overdoses has only continued to climb, even as drugs such as buprenorphine that can help overcome addiction and slash the risk of overdose are becoming harder to access than opioids themselves.

The twin problems of patients with a legitimate medical need losing access to opioids, while the addiction and overdose rates swell, add up to a new opioid crisis that may be worse than the original one that emerged at the turn of millennium. Federal and state governments, along with health care, bungled the response to that original crisis, say a range of experts.
As a result, patients and the addicted are caught between the pincers of prescription cutbacks and increasingly difficult-to-access options for dealing with addiction. "Pain was poorly treated in America up through the 1980s before we started paying attention to it," says Keith Humphreys, a psychiatry professor at Stanford University and a drug policy adviser in the Bush and Obama White Houses. "Today we're still failing."
Skyrocketing Overdoses
The National Institutes of Health reckons that more than 80,000 people died in America from opioid overdoses in 2021, the most recent year for which figures are available. That's roughly double the number in 2015, when synthetic opioids started to take off. Nearly a million people have died from opioid overdoses since 2000. Public health experts forecast another half-million deaths in the next 10 years.

The criminal prosecution of Purdue Pharma, owned by the Sackler family, over its zealous promotion of opioid products did much to bring the crisis to the public's attention. In 2007, three Purdue executives pled guilty to criminal misdemeanors and the company itself was prosecuted in 2020. The episode also left many people with the impression that the crisis was entirely the fault of Purdue and other pharmaceutical companies, who downplayed the addictiveness of opioids. But that claim is misleading.
Although pharma's aggressive, deceptive tactics were a big factor in the rise in addiction, the idea that opioid addictiveness was largely a myth, and the resulting drive to prescribe them more aggressively, originated within medicine itself. In 1980, findings published in the New England Journal of Medicine concluded that "addiction is rare in medical patients with no history of addiction." As a result of this and other research, doctors shifted their focus in the 1990s toward doing more to treat pain.
Those findings were badly flawed and now largely discredited, but not until opioids had been trumpeted prominently as nonaddictive wonder drugs in feature articles in Scientific American and Time magazine, and much of the media had followed suit. Doctors and hospitals readily embraced a new means for leaving pain-ridden patients feeling better treated.

"The Sacklers and Purdue have stolen the spotlight in the opioid problem, but there's plenty of blame to go around," says Andrew Kolodny, a physician and medical director of the Opioid Policy Research Collaborative at Brandeis University's Heller School for Social Policy and Management. "Researchers were downplaying risk and promoting aggressive prescribing. And we have a health care delivery system in which patients are customers, and that favors a quick fix like a prescription," he says.
Opioid makers and distributors have since faced a reckoning in the courts, leading to combined settlements of about $50 billion in the past two years—money earmarked for states to fund addiction prevention and treatment efforts. In 2016, the CDC moved to address the medical side of the problem. It issued new prescribing guidelines that called for making opioids a relatively rare last resort and for getting most patients who were on opioids off of the drugs. "The whole culture of prescribing opioids has radically shifted toward a crackdown on prescribing," says John Kelly, a professor of addiction medicine at Harvard Medical School.

Since the prescription cutbacks took hold, the number of opioid overdoses—the best and starkest measure of the damage done by opioid abuse—has skyrocketed in the U.S. The simple reason: street drugs.
Prescription opioids may have helped trigger the opioid crisis, but the ready availability of illegal fentanyl has sustained it. Fentanyl, the most powerful of opioids and the most profitable to smuggle and illegally sell because a small pill packs such a potent, if potentially deadly, punch, is mostly manufactured in China and smuggled into the U.S. through Mexico or South America.The big problem, as it turns out, was never really with patients who were legitimately prescribed opioids. Initially, in the early aughts, doctors were giving out prescriptions to too many patients, and prescribing each of them too many pills on average. But the dangerous fallout from that overprescribing wasn't that too many patients were becoming hooked and overdosing; it was that hundreds of millions of excess prescription pills were finding their ways to people who weren't prescription holders.
In 2016 the deputy director of the federal National Institute on Drug Abuse (NIDA) estimated that the pills of one in five patients prescribed opioids were getting into the hands of other people. More than 70 percent of prescription opioids that are abused were prescribed to someone else, according to a 2019 study of opioid use in Colorado. When the U.S. Drug Enforcement Agency began a campaign to recover unused prescription opioids in 2010, it gathered up more than 2,400 tons of pills over four years.
"It was 'the medicine cabinet problem,'" says Amy Bohnert, an epidemiology professor at the University of Michigan. "When there are that many pills being prescribed, some of them get diverted to curious teenagers and others, and some of those people will get addicted."
This misuse of prescription pills essentially introduced opioids to a huge population of people who were then using and abusing the drug outside of a doctor's oversight. Addiction and overdoses followed, but the misuse—and the problems associated with it—quickly shifted from prescription to illicit opioids.

The numbers make this point clearly. Illicit opioid usage accounts for nearly five times as many overdose deaths as prescription opioid deaths, according to the CDC. While opioid overdose deaths have been rapidly rising overall, those among prescription users fell from more than 17,000 in 2017 to just over 16,700 in 2021, according to NIDA, suggesting that the overall rise is entirely from illicit opioids.
Because the great majority of addictions and overdoses were occurring, and continue to occur, outside of the pool of legitimately prescribed users, sharply curtailing prescriptions hasn't solved the problem, given the now-widespread availability of opioids as street drugs.
Suffering Patients
Cutting back on opioid prescriptions has had a big unintended effect: It's made it increasingly difficult for legitimate patients with an ongoing medical need for treatment for severe pain to get relief from prescribed opioids. "The pendulum has swung too far back the other way in terms of everyone putting the brakes on pain medication," says Harvard's Kelly. Currently five million to eight million patients are prescribed opioids for chronic pain, according to the CDC. Those numbers are shrinking: A 2020 CDC study found that 22 percent of chronic pain patients had used an opioid within the past three months, versus a 2010 study that put the number at 36 percent. But it's not at all clear that the drop is for the best.

Experts are nearly universal in their agreement that patients with terminal or most advanced cancers should be able to get opioids. And yet data shows that fewer cancer patients have gotten opioid prescriptions in recent years, suggesting that even many of those patients are finding it harder to get prescriptions under the crackdown. "Everyone agrees these are appropriate cases for opioids," says Humphreys. "I was a volunteer counselor in hospice care, and I've seen what a fentanyl patch can do to ease the pain of a patient with bone cancer."
The denial of opioid access is even more widespread among other types of patients who in the past have generally been able to get prescriptions for chronic pain, notes Humphreys. These patients include those with nerve disorders, spinal conditions, sickle-cell anemia and later-stage multiple sclerosis. "The pain for patients with some of these conditions can be excruciating," he says.
Danny Barcelona is one of those patients. He was diagnosed nearly 20 years ago with fibromyalgia, a nerve disorder that can make even a gentle touch agonizingly painful. He has also needed two shoulder surgeries, and several spinal treatments, including laser treatments and injections. He has been on prescription Darvocet, tramadol and oxycodone—all forms of opioids—for most of the time since his diagnosis. On a few occasions his doctor insisted he try stopping, refusing to write prescriptions for a while. "Every time that happened," he says, "I thought I was going to die."
Barcelona says he would rather not be reliant on opioids. He has turned to dozens of other pain relief medications and treatments, from acupuncture to nonsteroidal anti-inflammatory drugs (NSAIDs) to magnetic stimulation, in the hope they would make it easier to cut back or even stop. They all either proved ineffective or had serious side effects—his doctor had to take him off anti-inflammatory pain relievers, for example, because they were damaging his kidneys.

Still, over time he has managed to reduce his intake of opioids from as many as five oxycodone pills a day to just two. In February, North Carolina passed a bill that would legalize medical cannabis, and he's hopeful that will open up a new pain-relief avenue. For now, though, he is terrified that he will be forced to stop opioids before he has a substitute treatment in place. "People who don't deal with this kind of pain don't understand how much energy it takes to combat it," he says.
Patients like Barcelona are chronic opioid users, meaning their prescriptions provide them with opioids for at least several months, and often many years. According to NIDA, these patients are considered "dependent" on opioids, meaning they experience withdrawal symptoms if they stop or cut back. But they generally aren't considered "addicted," which NIDA defines as compulsive drug-seeking and as continuing on with the drugs in spite of the large risk of harm.
Chronic prescription opioid users, in fact, tend to use the drug relatively safely.
The bigger risk comes in forcing them to cut way back or stop. Still, that is exactly what has been happening across the country in recent years. One large study found that reducing dosages increased patients' risk of overdose by more than 25 percent and of being hospitalized for a mental health crisis by about 75 percent. A second large study found that stopping their medications altogether made them about four times more likely to die by suicide. The studies weren't designed to determine why forced tapering or cutoff led to these grim outcomes. But to Kate Nicholson, an attorney who founded the nonprofit National Pain Advocacy Center, which does not accept industry funding, the implications are clear. "Forced tapering is highly destabilizing," she says. "It's dangerous." Even the authors of the 2016 CDC guidelines that recommended the cutbacks warned in 2019 in the New England Journal of Medicine that the results appeared to be causing "serious harm" to patients.

In response to the growing recognition of the risk to patients of cutbacks, the CDC revised its 2016 guidelines in 2019, easing its call for restrictions and warning of caution in reducing or stopping the opioid medication of chronic patients. That call for caution has largely been ignored. Reports in the media decrying the supposedly wanton and deadly addicting of millions of patients by negligent doctors acting under the influence of puppet-master pharma companies have persisted. (New York Times: "How the Sacklers Got Away With It;" Reuters: "'You got rich off our dead bodies'"; Fox News: "Overdoses continue to fuel sales for the Sacklers"). The finger-pointing encouraged state governments, courts, insurers, hospitals and doctors themselves to codify the cutbacks into regulation and standard practice.
In 2019 doctors in Wyoming and Alabama were sentenced to prison—25 years in one case—for prescribing opioids under toughened laws in those states. Those sentences were reduced in 2022 by a federal appeals court in one case and overturned by the Supreme Court in another. But the warning to doctors about the risks of prescribing opioids was clear. "The changes have had a chilling effect on care," says Nicholson. "It's left doctors afraid to prescribe medications to people who have been on them for years."
Worse, Nicholson adds, the crackdown has led insurance companies increasingly to refuse to pay for opioids. For less-affluent patients, it is simply another form of shutting off their access—or pushing them toward illegal opioids.
How to Cut Back
Where America needs to cut back on opioid prescriptions, agree experts, is in routinely prescribing dozens of pills for "acute" pain—that is, pain that remains severe for a relatively short period of time, as is often the case with patients who have surgery. For these patients, there may be no great need for an extended prescription of opioids, or in many cases for any opioids at all. "It might help to prescribe a small number of pills to help them get over that initial hump of pain, and then give them ibuprofen," says Kelly. "But we shouldn't be prescribing 30 or 40 pills to patients who aren't already taking opioids for chronic pain, which is what was happening in the past."

While the cutbacks have left chronic pain patients struggling to keep their prescriptions, they haven't stopped the routine prescribing of opioids for acute pain, says Kolodny, and that needs to change. He notes that the average number of opioid pills currently being prescribed for post-surgical pain is 20, while among all other countries with advanced health care systems the average is zero—even in the hospital, patients in most countries simply get NSAIDs. "It makes no sense that we do that," he says. "For most cases of severe acute pain, such as surgery or kidney stones, Tylenol plus an NSAID probably gives better pain relief." Yet even dentists still routinely prescribe opioids for an ordinary wisdom-tooth extraction, he notes, and studies show that one in eight patients who show up in emergency rooms with twisted ankles get opioids.
Unnecessary prescriptions for acute pain lead to addiction for some patients, but this is a tiny minority; a 2021 review study found the risk of addiction from prescription opioids was less than three percent, and that figure included chronic pain patients, suggesting the number for acute pain patients is lower. By contrast, the U.S.' opioid addiction and overdose problem is massive—and almost entirely driven by illicit use of fentanyl smuggled into the country. Studies indicate that four out of five people addicted to opioids never had a prescription for them; they started with illicit use, and continued on. Medicine and government is failing these users, too, say experts, by making it far too difficult to access treatments that have been proven effective in reducing overdose risks and making it easier to get off of opioids.
The three most effective treatments are methadone, buprenorphine and naltrexone, all FDA approved, and all of which are essentially slower-acting, milder opioids that fend of withdrawal symptoms and cravings, without providing the strong high that can intensify addiction and interfere with other aspects of living. They cut the risks of overdose by as much as half. "They're good medications that can lead to dependence but not addiction," says Kelly. "They're like wearing nicotine patches to reduce tobacco cravings."

People with opioid addictions are much more likely to beat their addictions and get off the drugs if they have access to addiction treatments, notes Bohnert. "There is evidence that the way the drugs are tapered can make a big difference. Slower is better, and so is adding in treatments and support."
But more than four out of five people addicted to opioids aren't receiving these treatments, according to a 2019 study published by the National Academy of Medicine. One reason is that federal law requires doctors to get special permission to prescribe buprenorphine and similar drugs, and face close monitoring when they do; in the current climate of fear about giving drugs to chronic users most doctors don't want to take the trouble or face the risk. For many of these patients, it is easier to get illegal fentanyl than a prescribed treatment drug.
Biden has promised to ease these laws and increase funding for treatment, and several federal laws have been proposed to support treatment access, including the bipartisan Modernizing Opioid Treatment Access Act now before the Senate and House. But so far there has been little to show for it, contends Nicholson. "The policy environment may be slowly changing, but it isn't filtering down to the lives of patients," she says, adding that health care is primarily regulated by the states, and most lag far behind in fixing the problems.
In addition to making it easier for clinicians to prescribe opioid addiction treatment drugs, state and federal policymakers can take other steps. For one, they could require more clinicians to get special training in preventing and managing opioid addiction, says Brian Hurley, president of the American Society of Addiction Medicine and an addiction physician. States could also enable Medicare and Medicaid payment for addiction treatment and ensure that incarcerated individuals are given more options for addiction treatment. "Restricting access to these tools is a threat to public health," says Hurley. "There's even a cost argument to be made, because while these programs can be expensive, they cost a lot less than a stay in intensive care for an overdose victim."
Treatment options could also be made easier to get. Making the overdose reversal drug naloxone freely available in vending machines in "hotspot" drug-misuse communities would increase the number of people who can get this treatment, says Shravani Durbhakula, a physician who heads pain education at Johns Hopkins Medical School and communications at the American Academy of Pain Medicine. So would placing clinicians who can prescribe treatment drugs at needle-exchange programs and setting up more mobile treatment clinics. The Food and Drug Administration could also more quickly bring new opioid treatments and alternatives to the market. "We need to lower the threshold for bringing help to people who need it," says Durbhakula.
Meanwhile, the overdose deaths and addiction misery continue to climb. "We need a new national strategy for treating, preventing and educating about addiction and pain," says Humphreys.
The question now is how many people will needlessly suffer or die before we get there.
Correction (5/5/2023, 12:52 EDT): This article originally stated, erroneously, that Purdue executives were prosecuted in 2020 over the company's promotion of opioids. In fact, only the company was prosecuted in 2020. Three Purdue executives pled guilty to criminal misdemeanors in 2007. The article has been modified to correct the error.