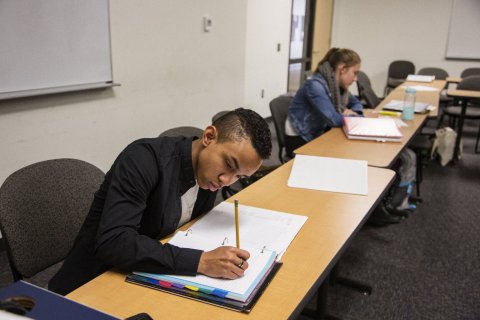
Updated | When Tai Jordan was a child, he would visit the local swimming pool and puzzle over why there were boys who splashed about without their shirts on, while he wore a bathing suit that covered most of his body. And when he thought about conventional weddings, he didn't understand what it meant to be a conventional bride or groom.
"I've never really identified with the body I was born in," says Jordan, an 18-year-old student at Evergreen State College in Olympia, Washington. "The way I decided to carry myself, the way I acted, was always more masculine."
Jordan initially identified as a gay young woman in 2013, but even after coming out about his sexual orientation, he still didn't feel "complete." He felt confused about the language used to describe what he was feeling. Jordan became an avid triathlete and threw himself into sports, which led him to an epiphany. During a soccer competition in his junior year of high school, he strained his quad muscles. When doctors performed an MRI of his lower body to diagnose the injury, they spotted something else much more serious. Next to Jordan's ovaries was a rare type of benign tumors, known as teratomas. Before surgery, the doctors discussed the possibility of having to remove his ovaries depending on pathology or what they found. Thankfully, they never had to. Jordan underwent a surgical procedure to remove part of one ovary. While it didn't affect his ability to have biological children, it prompted him to think more deeply about himself. During his post-op appointment with his doctor, his mom encouraged him to broach the topic of identity. The quest helped Jordan realize he wasn't gay. He wanted to become a man.
Announcing to the world—or just your family—that you want to transition to the opposite sex is almost never easy, and making that transition is always a long ordeal, physically and psychologically. Though it's a procedure that's slowly becoming much more accepted by the public and the medical community, the prospects are still fraught for a young person who may have been chided by adults for feeling trapped in the wrong body, or ignored. Families and pediatricians may insist it's just a symptom of the undignified phase of life known as puberty, or another bit of self-indulgent behavior typical for angsty teens.
Jordan's experience was much more positive. He came out to his mother a second time (first as a lesbian, now as transgender) and watched her tear up (again). "She wasn't crying because she was sad, she was crying because she knows the statistics, and she knows the reality of what happens to people in the LGBTQ community: the unprecedented rates of suicide, the ability to fall into depression, the lack of resources," says Jordan, who knows that around 40 percent of people who identify as transgender will attempt suicide as teenagers. These young people also have significantly higher rates of homelessness, substance abuse and depression, compared with the general population.

Jordan is one of approximately 700,000 people in the U.S. who identify as transgender, according to the Williams Institute, an independent organization dedicated to research on sexual orientation and gender identity. Thanks to greater awareness and acceptance, transitioning is now an option at an increasingly younger age. However, the medical interventions used—hormone treatments, drugs to halt puberty—are highly controversial. Critics argue that the treatments are unethical and that young people are not psychologically or emotionally equipped to make such a momentous decision.
Others in the medical community vehemently disagree, and they are working hard to normalize the process by providing these treatments at children's hospitals.
Jordan connected with Dr. David Breland, a physician of pediatric and adolescent medicine at Seattle Children's Hospital and director of its new Gender Clinic. Soon after meeting with Breland, Jordan began testosterone therapy. It caused him to develop certain characteristics associated with men. Breland specializes in working with transgender teens, and he has seen at least 200 young patients like Jordan. He helps families make sense of the process. He calls it a new kind of puberty, through which young people can grow into the adults they want to be. Advocates say going through this transition process early minimizes stigma and improves both the medical and cosmetic outcomes.
Seattle Children's Hospital is the fifth to open a clinic dedicated to the complex needs of this young patient population. Breland and his colleagues will see children and adolescents ages 8 to 21, offering a high level of care that include specialists in endocrinology and behavioral medicine. At the Seattle clinic, children will also have access to psychological counseling. They may also be provided with pubertal blockers to "buy the family some time" before starting a child on cross-sex hormones at the onset of puberty, says Breland. Though the hospital isn't doing reconstructive surgery to alter the appearance of genitals or the chest, it does provide guidance and referrals if a patient wants to undergo surgery later, most likely after reaching the age of 18. Experts in this specialized field say it's clear that transitioning earlier in life can result in fewer medical procedures as an adult. Hormones administered in early puberty can prevent a person's features from becoming too masculine or feminine, and the process is much less painful than the often drastic and costly cosmetic surgery some patients require to look the way they see themselves. Early transition, some say, also results in improved mental health.
But Breland knows the timing is different for every patient. "There's a lot of risk factors that happen with these people, and they just want to be themselves," he says. "That's why we think it should be a team effort, with a medical provider and a mental health provider so they can use psychotherapy and mental health evaluation to make sure it's the right decision for them."
Better to Have Cancer?
Most doctors in this growing specialty follow established protocols for early transition. The World Professional Association for Transgender Health, a nonprofit, provides education and training for physicians to learn about caring for this patient population. It also advises the growing number of children's hospitals offering these services on standards of care for transgender patients.
Other, more mainstream medical organizations have also weighed in. The American Academy of Pediatrics, for example, recommends physicians and adults have the first discussion about transitioning when the child is 12, but the organization believes the process should start at 18.
Though advocates in the field have their own ideas about when to start the process, not enough is known about the factors that prevent transgender patients from receiving the right kind of care. Breland recognized this and conducted some research before starting his clinic. For the study, published in the Journal of Adolescent Health, he and his colleagues interviewed 15 transgender patients and 50 caregivers to learn more about the challenges they faced when seeking care. They identified several big issues. Some participants said it was hard to find pediatricians trained to provide "gender-affirming health care." Others reported a lack of consistently applied protocols for handling these patients. Some said they encountered clinicians who failed to coordinate care or limited and delayed access to pubertal blockers and hormones. It was common for doctors to inconsistently use chosen names and pronouns. Breland says his research proved that "it's easier to have a chronic medical condition" than to be transgender.
When treating his youngest patients, he prescribes pubertal blockers that halt puberty altogether and prevent the development of biological sex characteristics. These Food and Drug Administration-approved medications, known as GnRH agonists, were initially created to treat precocious puberty (when a child begins puberty before 8 or 9). The hormone in the drug overstimulates the gonadotropin-releasing hormone receptors in the brain, and "it just shuts these receptors down," says Breland. The effects are mostly reversible if a patient stops taking the agonists.

When the patient and family feel ready, the clinic will move forward with the transition. Breland says most decide to, and he then prescribes the cross-sex hormone—testosterone for transmales and estrogen for transfemales. This usually begins when doctors determine the child has started puberty. Adding these drugs allows patients to begin developing into an adult of their reassigned sex. "Just like someone going through puberty, their testosterone or estrogen will gradually increase, and that's what changes the body and voice and hair growth and breast development," says Breland. He prescribes a gradual increase in dosage so levels of estrogen or testosterone will rise in the body, as they normally would for an adult who is biologically female or male.
Taking the hormones affects a number of the person's physical traits. When boys transitioning to girls take pubertal blockers they won't develop biological sex characteristics such as bigger stature, a broad face, larger hands, an Adam's apple and a deeper voice. Girls transitioning to boys will develop some traditionally male characteristics, such as facial hair. A biological female in this protocol usually stops menstruating after six months. Transitioning to a male will cause the patient's voice to become deeper, and that's likely to be a permanent change. The hormones don't change the overall appearance and function of a patient's genitals, but testosterone may cause an enlargement of the clitoris, which can be useful should the patient want to have genital reconstruction later in life, says Breland.
Jordan began taking testosterone to transition from female to male in 2014, during his senior year of high school. He now administers his own testosterone shots every other week, and it will be something he does for the rest of his life. He says the process feels like a "second puberty." The difference this time is that he welcomes the changes in his body. "You've got the acne, the facial hair, the voice cracking at weird points in the day," he says. "These are the secondary sex characteristics I would have liked to have happened initially."
Dissing Dysphoria
Up until 2012, the American Psychiatric Association listed "gender identity disorder" in the Diagnostics Statistical Manual of Mental Disorders, which suggested that patients who questioned or felt troubled by their biological gender were abnormal. In 2012, after decades of classifying transgender people as mentally ill, the APA replaced the term with "gender dysphoria," which is used to describe the distress felt by some patients about this aspect of their identity. It essentially affirms that gender nonconformity isn't a psychiatric illness.
This change in the field of psychiatry has has helped to bolster an area of medicine within a subspecialty of endocrinology. And while there's an increasing demand for trans-friendly physicians, there aren't enough specialists who are fully qualified to handle their medical needs. A new study published in the Journal of Endocrinology & Metabolism found four out of five endocrinologists have never received formal training on care for transgender patients. Additionally, a majority—80 percent—of the 411 physicans that took part in the survey said they'd worked with a transgender patient at some point during their career but without a specialized education.
But while many physicians hail that change, others think it's dangerous to make it easier for young people to rush into transitioning. Dr. Lawrence Mayer, a resident in the department of psychiatry at the Johns Hopkins University School of Medicine and a professor of statistics and biostatistics at Arizona State University, argues that young people aren't equipped to make these judgments for themselves. Kenneth Zucker, a researcher at the University of Toronto and a therapist, suggests in several journal articles based on studies he conducted that early traumatic experiences with family, such as an absentee parent, can bring out gender-nonconforming behavior—but these feelings eventually go away. His research suggests that as much as 90 percent of the children who identify as transgender eventually accept their biological sex after puberty. In a follow-up study of 25 transgender biological females, he found that only three still identified as transgender in adulthood. Zucker used his research to formulate his own approach to treating these patients. His treatment is controversial because he focused on helping a child become more comfortable in his or her body, rather than getting the care needed to transition early.
Mayer and others believe early intervention shouldn't include drugs. Instead, it should focus on encouraging young people to experiment with their gender in ways that are more mutable. This may include changing hairstyle and clothing and using a different name. "I would be happy if these children would be sent to general child psychiatrists and followed for a period of time without their parents being there and see what they believe and how persistent it is," he says. "If it's persistent enough, I would be supportive of them because I care about patients."
Mayer co-authored a report that argues more data is needed to understand the outcomes of early transition. The problem, he says, is that very few balanced studies have been conducted, especially on early intervention. His paper cites one study, published in Pediatrics, that found that reassignment surgery in young adulthood alleviated gender dysphoria, and that the well-being of these patients was similar or better than young adults in the general population. But Mayer says this study wasn't well-designed—it was based on only 55 transgender young people and didn't have a matched group of transgender patients who didn't undergo medical treatment.
Jordan doesn't feel as if he needs studies to affirm his experience. He would strongly disagree with Mayer's watch-and-wait approach, which he believes simply reflects a misunderstanding of the situation. "If it's going to take a little poke or a pinch or some soreness to feel better, to feel happy and to be able to move on with my life, then it's a mere hiccup in the rest of my life," he says. "Nobody knows your body better than you do."
Even if it turns out to be the wrong one.
Updated: This story has been updated to reflect Jordan's comments on statements provided to Newsweek during initial interview.
Correction: The story has been updated to clarify that pubertal blockers, not sex hormones, prevent a boy from developing biological sex characteristics.
The story has been updated to clarify that a doctor will prescribe cross-sex hormones when it's determined that the patient has started puberty.