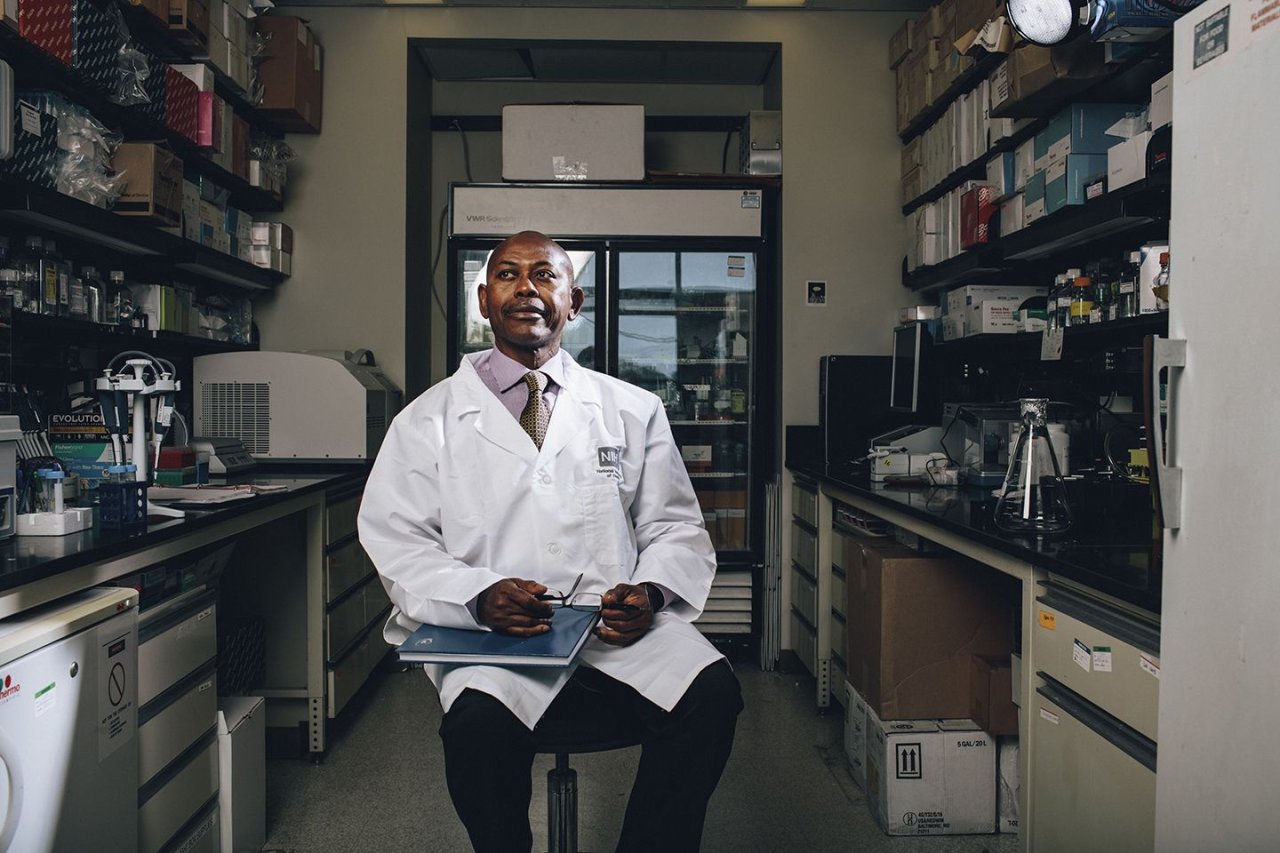
Charles Rotimi first realized the future was passing him by around 2005. The Human Genome Project had recently finished spelling out an entire set of human DNA. Following that breakthrough, scientists in six countries across the globe had begun collecting blood samples to find genes responsible for various conditions, including serious diseases, which could lead to treatments. And Rotimi, who was leading that collection effort in Africa, had the sick feeling that history was repeating itself.
He wasn't concerned about himself so much as his homeland. In the past, African patients have had poor access to medical advances, even as scientists use them as research subjects. Rotimi worried that genetics might again exploit the 1 billion people n sub-Saharan Africa, ignoring their need for treatments for HIV, tuberculosis, malaria and cancer. "The genomic revolution was going to fly over Africa," he says, "and tomorrow's medicine will not work for all."
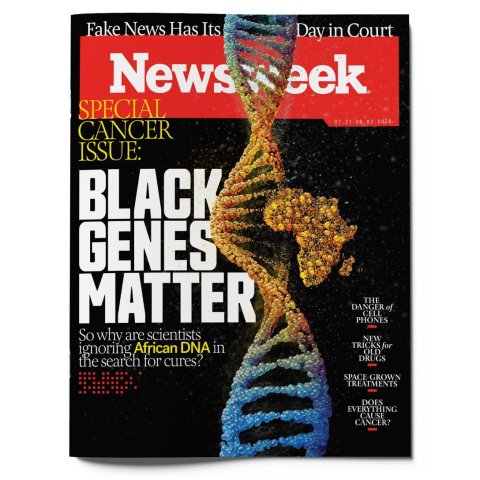
His concern was well founded. Over the next few years, scientists came out with a frenzy of discoveries about our DNA that could possibly lead to new treatments for diabetes, cancer, psychiatric illnesses and other serious diseases. But they were drawing from a small slice of the world: Nearly all of the published work was based on populations with European ancestry. By 2009, fewer than 1 percent of the several hundred genome investigations included Africans.
The genomics revolution soon began to sputter. Being able to know the exact genetic makeup of each patient was to bring a new era of treatments tailored for each individual. But doing so depends on finding minute variations in our DNA that correlate with the occurrence of disease or bad drug reactions. This task requires the full range of genetic variation among as many humans as possible. Otherwise, genomics research is like a search party that circles the same few trees looking for signs of the killer rather than spreading out through the entire woods.
The richness of African genomes is a product of the evolution of our species. Modern Homo sapiens originated in Africa about 200,000 years ago. About 100,000 years later, 1,600 or so men and women—from a population of at least 20,000 and likely much more—left the continent and spread around the globe, eventually reaching Europe and, more recently, the Americas. "In other words," wrote University of Washington geneticist Mary-Claire King and colleagues in a 2017 commentary, "about 99 percent of our evolutionary experience as a species was spent in Africa."
Whatever genetic diversity existed across the continent until then was almost entirely left behind when that small group emigrated—and it is there still, hidden in the genes of each African. That is partly why Rotimi was so dismayed by the exclusion of Africa from genomics. "We are all Africans beneath our skin," he says.
More and more scientists are coming around to Rotimi's view—that Africa contains one of the greatest weapons in the quest to combat cancer: the DNA of its people.

Unpacking the Genome
As a Nigerian-born scientist specializing in genetics and health disparities, Rotimi foresaw the consequences of omitting Africans from genome studies years before many other researchers even noticed. And he was uniquely positioned to do something about it.
Born in Benin, Nigeria's fourth-largest city, Rotimi first saw health inequalities in a big way in America. He came to the U.S. for graduate school at the University of Mississippi, where many of the state's wealthiest families send their children, a trip that introduced him to his first Big Mac. "I just couldn't eat it," he recalls. "I couldn't fathom the concept of bread, meat and leaves together."
Worse was the taste of inequality he got while traveling around the state. "That is when poverty speaks very loud, when you are in an environment with a lot of resources, but you don't seem to have them," he says.
He returned to Nigeria armed with a graduate degree. But after six months of job searching, he had yet to find an opportunity to do the research he knew was needed. He returned to the U.S., eventually earning doctorate degrees in public health and epidemiology.
Those years deepened his awareness of the importance of genes to health. Life in Nigeria had already shown him that sickle cell disease was fated by birth, not by upbringing. Now, his research on hypertension among Africans around the world showed him that although lifestyle and the environment shape health, so does DNA.

As Rotimi was appreciating the power of genetic inheritance, scientists were on their way to sequencing the first human genome. Tightly coiled inside the nucleus of every human cell, the genome consists of about 20,000 genes that encode proteins guiding the multitude of biological processes happening all the time in our bodies. Genes, in turn, are made of DNA, helical strands of compounds called nucleotides that contain chemicals called bases. These four different bases—known most commonly by the initials A, C, T and G—are the language of the genetic code that makes up each unique individual's blueprint. A human genome—that is, the complete set of a person's genes—consists of 3 billion bases.
The Human Genome Project, which was completed in 2003—by then, Rotimi was teaching microbiology at Howard University, in Washington, D.C.—sequenced most of a single person's genome. The breakthrough wasn't so much the sequence itself but the technology. If research could match diseases or drug reactions to errant genes, doctors could tailor treatments around the unique genome of each patient. To arrive there, though, scientists had to study the small ways a genome varies from one person to the next. The tiny fraction of our DNA that differs, researchers thought, had to be responsible for many inherited conditions. What they needed to study was not one genome but many.
They were looking for changes to single bases—a mutation from an A to a C, or a G to a T—among the 3 billion in a human genome. These can occur when DNA replicates, either when a baby is conceived or as cells divide during our lives. These swaps, called single nucleotide polymorphisms (SNPs, pronounced snips), are often harmless but sometimes alter how a gene works, raising the risk for certain diseases. The wrong SNPs can render people more susceptible to Alzheimer's, some blood diseases, male infertility and cancer, among other conditions. And once they're in the genome, they can be passed to the next generation.
Precision medicine is based on the idea that finding a culprit SNP can lead to treatments targeted against the gene in which that SNP sits. To find SNPs, researchers conduct association studies in which they compare whole genomes of many people.
After the Human Genome Project was done and the cost of sequencing genomes came down, these genome-wide association studies picked up the pace. But they suffered from a diversity problem: Almost none of them included African genomes.
When those first few people left Africa 100,000 years ago, they took their inherited SNPs along with them. But they left behind an enormous amount. And the larger population that remained in Africa meant more genomes churning out variety, generation upon generation. Because the ancestral trees of Africans have been branching out for so much longer than those of Europeans and Americans, they contain much more variation. In fact, African genomes are the most diverse of any on the planet.
"We compared European and Asian populations to each other," says Sarah Tishkoff, a geneticist at the University of Pennsylvania, "and they were more similar than any two African populations we looked at." When it comes to genetic diversity, Africa has a 100,000-year head start.

The Perils of Exclusion
Including Africa in the search for problematic SNPs has several crucial advantages. SNPs involved in diseases like cancer are usually rare, and a rare SNP found in the genome of someone with cancer could lead a researcher to link the two. But what seems like an uncommon mutation among European genomes may turn out not to be when Africans are added to the mix, says Nicola Mulder, who analyzes genetic data at the University of Cape Town in South Africa. That mistake could waste years of effort and lots of money.
A group of scientists once presumed that five genetic variants caused a dangerous thickening of the heart, even going so far as to tell people with those variants that their DNA put them at risk for cardiac troubles. But they were wrong. Those five variants were not rare at all and in fact completely harmless. If the scientists had included African populations in their work, they might have known.
More important, compared with Europeans and Americans, Africans have much better genomes for research, again because of their ancestral age. Over time, as a genetic material is handed down from one generation to the next, SNPs tend to gather in clusters, making them easier for researchers to find. As a consequence, they are more apparent in older genomes—in other words, African ones. "That can be of use to all populations," says Tishkoff. For example, this clustering phenomenon led geneticists to a gene associated with LDL cholesterol (the bad kind) and another related to inflammation.
African genomes have been rubbing up against environmental threats for far longer than any others, forcing the appearance of some surprising traits that may hold vital clues about disease. A genetic mutation that enables us to survive one hazard may also shackle us with a less harmful new trait. Take sickle cell anemia: The gene behind this condition also protects against malaria. Another mutation makes people immune to the parasite behind African sleeping sickness but also increases their risk of kidney disease.
It's not hard to imagine, Tishkoff notes, a mutation that enabled people to survive some menace but also left them predisposed to cancer. Though the menace disappeared—say, in the move from East Africa to North America—the variant remained. These relic mutations could help explain how or why cancer evolved. "Given the vast genetic variation that exists in African genomes," Rotimi says, "it is likely that we can find genetic variants that are important to cancer that may not be discovered from other human populations."
And just as African genomes can help us recover our collective past, they can also save us from a perilous future. Some genetic abnormalities influence how our bodies respond to medications, a field known as pharmacogenomics. One variant, for example, leaves people with HIV less tolerant to an anti-retroviral drug, a discovery that is changing treatment regimens across sub-Saharan Africa. Another messes with the breast cancer drug tamoxifen. The more diverse the genome, the higher the odds of finding mutations that may shape the choice of medication.
"Increasing genomic research in Africa is going to benefit not just people of African descent," Tishkoff says, "but all people."

Correcting a Major Tactical Error
Even before the Human Genome Project was done, RotimI suspected Africa was being left behind. In 2002, he was an epidemiologist at the National Human Genome Center at Howard University and led the African branch of a project to collect genomes from around the world to uncover the scope of human genetic variation. Already, African scientists had a limited role, which stung Rotimi.
In 2004, while directing the Genome Center, he became the founding president of the African Society of Human Genetics, an organization formed to address this concern. At the group's first meeting, held in Ethiopia in 2006, the lack of participation by Africa—both its DNA and its scientists—in genome research dominated the agenda. A year later, geneticist Francis Collins, who led the Human Genome Project and now directs the National Institutes of Health (NIH), attended the second meeting, held in Cairo, where the concern began morphing into an idea for an Africa-based genome project.
Rising rates of cancer on the continent added further urgency. The prevalence of breast, prostate and cervical cancers is increasing there, partly due to lower mortality rate for infectious diseases and partly due to a shift toward a Westernized lifestyle. Current estimates put Africa's annual cancer incidence at 1.27 million by 2030. The problem is compounded by African patients being treated with drugs tested on non-African populations. Including African DNA in genetic research could ameliorate that issue. "How can I explain that a tool this robust," Rotimi asked himself, "is just going to pass by Africa in a way that will exacerbate already bad health conditions in this part of the world?"
The 2009 report exposing the paucity of African DNA in genome studies began spreading the alarm Rotimi had been sounding for years. The National Human Genome Research Institute, part of the NIH, began monitoring the over-representation of people of European ancestry in these investigations. "Far too much of the research we've done has been on people who are of most immediate European descent," says Eric Green, who directs the institute. He refers to this bias as "a major tactical error." That same year, Rotimi took the first steps toward a project that would not only correct that error but also transform a continent of scientists.
In 2010, the NIH began funding Rotimi's effort to organize a project focused on African genetics. If the West wouldn't include Africa in its work, he and his colleagues decided, they would do their own studies. But Rotimi quickly realized that an Africa-centric effort had to do more than collect sequences and catalog SNPs. The rare appearance of funding for such research, coupled with the desperate need for better medical care, made practical application of the work a priority. And he was haunted by the specter of past research testing medicines and techniques on Africans but never helping them. "We needed to be very careful," Rotimi says, "that the money addressed issues that are important to African people."

As he envisioned it, the project, which Rotimi eventually named Human Heredity and Health in Africa, or H3Africa, would do far more than study African genomes: It would be a massive research effort led by African scientists, located in African institutions and directly benefiting the African population. H3Africa would create parity between researchers there and in Europe and North America. A geneticist in Nigeria could compete with one at Harvard for funding—and win. Such an approach would avoid the disheartening patterns of the past and instead directly benefit African communities. In short, H3Africa would not just ensure that the genomics era landed squarely on the continent but that the kind of omission that characterized its early years would never happen again.
The NIH and the Wellcome Trust, a private charity based in the U.K., agreed to fund H3Africa for two five-year cycles. With the first cycle of funding—$76 million—H3Africa established 29 research centers across the continent, including in Sudan, Sierra Leone and Ghana—countries rarely associated with science before now. A cervical cancer project is collecting genomes from 12,000 women in several countries to better understand the mutations that raise the risk of human papillomavirus triggering the malignancy. At South Africa's University of Witwatersrand, geneticist Christopher Mathew is studying a kind of esophageal cancer common in Africa but rare in North America, and therefore neglected by research.
"It's been very difficult to do anything like this in the past," he says, "given the weakness of our local currency." The 10 years of funding will total nearly $190 million.
But the vision of a genetics project free from ethical dilemmas has not proved easy to achieve. Using money from non-African countries to fund research and the permitted inclusion of non-
African collaborators in H3Africa-funded projects raises several concerns. "Some ethics committees in Africa," says Jantina de Vries, a bioethicist at the University of Cape Town, "seem to believe that international collaboration is always exploitive." For decades, experts from the U.S. and Europe have come to Africa, taken what they needed and left, a practice aptly nicknamed helicopter science.
About 10 years ago, for example, an international group of geneticists took DNA samples from the eldest members of four communities of San, hunter-gatherers in southern Africa with the oldest known lineages on Earth. "That project really did come, take samples and leave," de Vries says. San leaders were furious that they weren't asked for permission, which they found disrespectful.

African scientists often end up with little involvement in the work using biological samples that they helped obtain. African patients often can't afford the drugs created with the help of their blood, spit and tissue. That history has left many researchers and would-be study participants skittish about genetic research. They worry that Africa will become an entire continent like Henrietta Lacks, the African-American cervical cancer patient whose family never knew that her cells had been exploited by scientists and widely used in medicine.
Collaborators, though, aren't always so ready to relinquish their position as the superior partner. De Vries, who chaired the H3Africa working group on ethics for several years, heard some international scientists argue that sub-Saharan Africa wasn't equipped to do sophisticated genetic research on its own. This perspective may have some truth to it, but it also maintains the status quo. "People and institutions that are powerful benefit from the perpetuation of that narrative," she says. "Those people are not interested in the substantive development of African research capacity."
Rotimi is trying to change that narrative. He wants to give African scientists the capability to stand on their own. A central tenet of H3Africa is to build the infrastructure necessary to support research that is just as worthy of the world's attention as that coming out of the best universities in Europe and North America. Toward that end, lead investigators on any H3Africa project must be African, and ideally the collaborators as well.
That requirement is building a new world of research capabilities across the continent, such as powerful computers to do bioinformatics research in Sudan; a repository in Uganda for storing DNA and generating a huge amount of data on the SNPs that protect against sleeping sickness; and equipment for fieldwork-documented hereditary neurological disorders in Mali, along with a laboratory to identify genetic mutations that increase risk and training for physicians there to educate Malians about genetics and disease. When the grants end, the new capacity remains for future scientists, "so that everybody doesn't end up like Charles Rotimi," he says, "who wanted to stay in Nigeria but couldn't."
These breakthroughs don't ameliorate all the ethical conundrums, though; fears of helicopter science persist. H3Africa encourages collaboration among countries within Africa, but those with less advanced research capacity hesitate to assist more polished countries. In Ghana, some scientists at poorer institutions resent those at wealthier ones presenting work on shared samples without acknowledging their contribution. Others say they sometimes have more input on samples sent to New York than to South Africa. "It's the same issue," says University of North Carolina bioethicist Eric Juengst. Just as with international collaborators, the idea of sending tissue samples across a border raises fears of exploitation and resentment about helping an economic competitor.
H3Africa has tried to allay the concerns by letting scientists own their samples for longer. International standards of genetic research dictate that data be made publicly available. But H3Africa gives scientists 23 months of exclusivity, so they can study and publish their data without competition. Publications increase the profile of scientists, making them more attractive to funders, which in turn enriches their country. Biological samples are protected for even longer. "For three years," de Vries and colleagues wrote in a 2015 paper outlining the program's policies, "samples can only be used for research that strengthens African research capacity."
Still, protecting scientists from competition doesn't necessarily protect patients, the hardest-hit victims of past exploitation because they gave their tissue and needed better medical care. Ethical guidelines for genetic research—these vary country to country, and H3Africa has its own strict regulations—say patients must give informed consent when they donate samples. But most languages across Africa lack words for technical terms like gene or biopsy.

Attempts to cross the language barrier haven't always gone smoothly. One well-intentioned scientist created educational material using eye color to explain heredity—this on a continent of people with brown eyes. And if the information is too technical, says Ogechukwu Ikwueme, who conducts H3Africa-supported breast cancer research at Nigeria's University of Abuja, patients shut down.
Gender dynamics and community hierarchies also impede consent. These problems pervade scientific research everywhere. But in Africa, poverty, low education levels, poor access to health care, language barriers and cultural restrictions amplify the concern. Rotimi often wrestles with questions about the women enrolling in his studies. "Is she participating because her husband has said so," he wonders, "or is she actually doing it on her own?"
Tackling that problem tugs at the heart of what H3Africa could mean—for the continent and for science as a whole. As de Vries sees it, reconceptualizing Africa as a land of scientific excellence "depends on what you think scientific excellence is." African laboratories may never sequence a genome in 24 hours. That playing field, Rotimi says, "is not really ever going to be completely level."
But excellence doesn't need to be restricted to technological savvy. "What African researchers are far better at," de Vries says, "is understanding patient needs and community needs." Ikwueme's breast cancer patients want to tell her about their lives and feel that she cares; otherwise, they aren't comfortable participating in research. And many traditional African communities prioritize the group over the individual, which means a patient's community often needs to be consulted about, say, study participation. "If I actually want to get the best from these patients," Ikwueme says, "I need to be involved."
Whether Rotimi succeeds in bringing about the change he seeks is uncertain. The program is now in its last funding cycle, and its scientists will need to start competing for grant money with the rest of the world. They also need government support, which so far has been in short supply. Rotimi has appealed to the World Bank for help, and a new office for handling grant applications, to be peer-reviewed by Africans, is now operating out of Nairobi, Kenya.
Researchers everywhere are at the mercy of government, but it's particularly challenging here. So far, country policymakers across sub-Saharan Africa have been reluctant to see the value of the work and agree to put more money toward science. Rotimi, who is now 61 and considers H3Africa a lifetime achievement, is well aware that politics could sabotage the whole effort. "Bad government," he says, "is probably the number one risk factor for health in Africa."
It is also poses a larger risk. A 2016 study examining whether genome research has become more inclusive of African DNA since 2009 found only a 3 percent increase. Of the 2,511 genome-wide association studies completed at the time, just 19 percent included minorities. "It wasn't surprising," says study author S. Malia Fullerton, a bioethicist at the University of Washington, "but it was rather shocking." The future of medicine depends on changing that history.