I remember being surprised the first time I saw it. It was bright white and as small as a tic tac but round instead of oval. My oncologist assured me I'd be thanking her in a few months.
As someone who had had painful periods since the first one I ever got, she said: "This medication will make all that go away."
That first day, I popped the pill into my mouth and swallowed it down with a sip of water. Tamoxifen was not just a pill that might help make my periods less painful. Starting to take it was, more importantly, the conclusion to my breast cancer experience.
After being diagnosed in April 2020, I had gotten through surgery and radiation during the worst of COVID-19, and was grateful to be "in the clear."
The hard part was over but, like 70 to 80 percent of breast cancer cases, mine was hormone-receptor positive, which essentially means the cancer cells feed off a certain hormone.
So, for me, that meant a five-year course of the estrogen-blocking medication Tamoxifen as a long-term treatment to prevent reoccurrence.

It wasn't long after I took that first pill that a new sensation began to take hold—my body felt like it was on fire.
As a 47-year-old, perimenopausal woman, I'd had hot flashes before, but this was of an intensity unlike anything I'd ever experienced and, even worse, it was not a flash at all. This seemed to have no end. Still, I thought, maybe my body just needed time to adjust?
And then I started to notice something else: I was crying—all the time.
It was as if suddenly I had an entirely different emotional toolkit than I'd had for all of my adult life. Things that previously would have been small stressors became a jumping-off point for uncontrollable thoughts of uncertainty and rumination. Bigger worries felt insurmountable. Was this normal?
Eight months after finishing treatments and taking my first dose of Tamoxifen, I was sure of four things. One, the hot flashes had gotten better or I was so used to them, that I didn't notice as much. Two, my doctor had been right about my period; the cramps were better. Three, I was not emotionally the same person.
And four, because of that, I was having a mental breakdown.
I kept thinking back to a few months before. At every doctor's office, I was handed lists of instructions, rules to follow, and told what to expect. The first of an endless array of gifts of encouragement I received just after being diagnosed, was a six-pack of socks with things like "brave," "warrior," and "courage" written across the toes.
Sitting in exam rooms, I'd stare down at my feet, read those words, and do my best to embody what they said. Other days, I'd tell myself not to think and repeat a mantra, "just keep swimming, just keep swimming, just keep swimming" over and over again. If I could just get to the other side, it would all be over, and I could go back to my life.
Through 21 days of radiation treatments, I made friends with the two technicians. In between telling stories about our children, one of them would invariably ask, "How are you today?" and I knew I could tell him the truth.
"The radiation burn is killing me and I'm exhausted," I replied on one of those days.
"You're almost there. You can do this," he assured me.
And then it ended, and I was on my own. No scripts to follow, no socks, no follow-up conversations with the people who had been in it with me. All of those things had gotten me through the during parts of breast cancer but what I hadn't anticipated, was the after.
I didn't know that even if I made it out okay, I still might not be okay. What was wrong with me? Shouldn't I just be happy it was over? Shouldn't I just be grateful that, unlike so many others, I was lucky enough to be on the other side?
Friends would ask: "But you're good now, right?"
I'd tell them what I thought they wanted to hear: "Yes, my scans are clear."
What I didn't tell them was in the weeks leading up to the scans, I was so riddled with anxiety I could barely cope with day-to-day life. Or that this little white pill I had to take to prevent the cancer from coming back had turned me into a person I barely recognized and exacerbated every mental weakness I possessed.
Or that my PTSD and fear of recurrence was so bad, I was barely sleeping most nights. Or that ever since I had cancer, every doctor I had gone to had run additional tests or scans because I was now in a different category than someone who didn't have that word on their medical records.
"With your history, it would be best to make sure," they would say. What I wanted to ask was, how was I now a person with a history? On paper, it made no sense. For decades, I had never been to a doctor for anything more than a sinus infection. Genetic testing showed I had no links to cancer.
I ran 20 miles a week. I ate a healthy diet. And now, I had my body back, but the question that kept circulating through my thoughts was, would I ever mentally be the same?
I spent almost a year stuck in this limbo until one day, I found myself sitting on another doctor's table begging for help. "You don't have to do this alone," she said. A week later, I started therapy.
It has been two years since then. I have had progress and setbacks. I have learned that many breast cancer patients struggle with side effects from medication and the emotional aftermath of having cancer.
Sometimes now, when I'm dressing, I catch a glimpse of my lumpectomy scar in the mirror, so faint unknowing eyes might not even notice it. I think about the day just after surgery when the bandages were removed. As they were slowly peeled away, I was so scared to see what was beneath, I had to force myself to look.
There, on the outer side of my left breast was a puckered slice, red against the ivory white of my skin. Seeing it made it real, tangible. But over the months, as I watched it fade, I knew my body was healing.
My emotional wounds may have been invisible but they were there, too and I needed to acknowledge them in order to move forward. And slowly, through endless boxes of tissues and a therapist who once a week allows me to tell her how I really am, I am.
These days, more often, I find a new mantra running through my mind: "I'm alive, I'm alive, I'm alive."
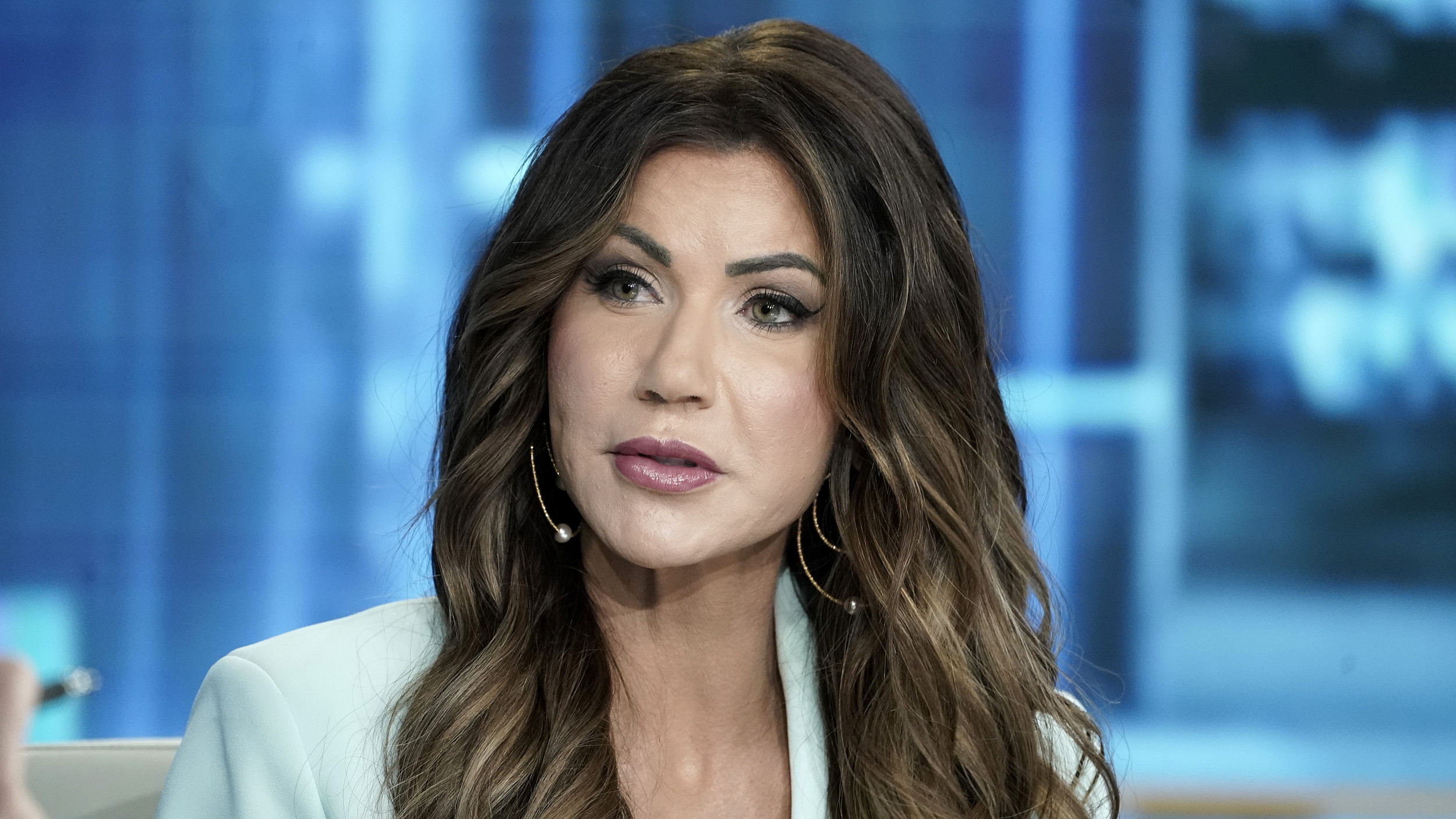
Darcey Gohring is a freelance writer and editor. She is the host of Zibby Mag Online Writing Community and a writing instructor. She specializes in personal narrative and memoir. Her work has appeared in Newsweek, HuffPost, Business Insider, Scary Mommy, and more.
She was a contributing author to the anthology, Corona City: Voices From an Epicenter, where she shared her experience of being diagnosed with breast cancer in the first few weeks of the pandemic. Darcey leads writing workshops and has served as the keynote speaker for conferences all over the United States.
All views expressed in this article are the author's own.
Do you have a unique experience or personal story to share? Email the My Turn team at myturn@newsweek.com.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Darcey Gohring is a freelance writer and editor. She is the host of Zibby Mag Online Writing Community and a ... Read more