Doctors have published photos revealing the disturbing impact of a dangerous fentanyl additive on the human body.
The images show the injuries suffered by a man in his 30s who had been injecting the synthetic opioid fentanyl adulterated with xylazine into his neck and arm veins for three years.
According to a case study published in the New England Journal of Medicine (NEJM), the man had presented to the emergency department with a one-month history of enlarging chest wounds.
Xylazine—also known as "tranq" or sometimes referred to as the "zombie drug"—is a medication approved only for veterinary use to sedate animals such as horses and dogs. The drug reduces pain and relaxes muscles, while also lowering blood pressure and heart rate.

In the United States, xylazine is increasingly being mixed with illicit drugs such as fentanyl, doctors and study authors Jessica O'Neil and Steven Kovach at the Perelman School of Medicine at the University of Pennsylvania told Newsweek.
Xylazine is most prevalent in Northeastern cities in the U.S. but it has been identified in illicit drug supplies in 48 states. And in Philadelphia, for example, xylazine was found in more than 90 percent of illicit drug samples tested in 2021, O'Neil and Kovach said.
Fentanyl is already a powerful drug with a high potential for overdose—which can be life-threatening. The drug is approximately 100 times more potent than morphine and 50 times more potent than heroin as an analgesic, according to the U.S. Drug Enforcement Administration.
But the combination of xylazine with the opioid is even more potent than fentanyl alone. While taking the two drugs together may produce sedation, pain relief and euphoria, both xylazine and fentanyl also lower heart rate, blood pressure and breathing rate, leading to the risk of overdose and death.
While the drug naloxone (sold under the brand name Narcan) can reverse the effects of fentanyl overdose, it has no effect on xylazine.
Drug overdose deaths involving xylazine are on the rise, data from the Centers for Disease Control and Prevention (CDC) indicates. From 2018 to 2021, the number of drug overdose deaths involving xylazine grew from 260 to 3,480 people, CDC figures show.
As the effects of the drug combination wear off, people can experience symptoms of xylazine withdrawal. These include discomfort, anxiety, insomnia, elevated heart rate and elevated blood pressure. In conjunction, they may also experience fentanyl withdrawal symptoms, such as pain, diarrhea, nausea, vomiting, fever and chills.
"After repeated use fentanyl and xylazine people can experience withdrawal, which can be difficult to treat requiring close observation and slow tapering of supportive medications," O'Neil and Kovach said.
Xylazine use is also associated with development of severe ulcerations of the skin, or so-called "necrotic wounds"—as can be seen in the images of the man in his 30s.
"We think that xylazine causes injury to blood vessels in the skin leading to the death of skin tissue and the development of slow-healing or non-healing wounds," the authors said.
Usually, these wounds appear on the arms and legs and do not always occur at the site where someone has previously injected. The wounds can vary in size, sometimes involving underlying muscle or bone. They can become infected with bacteria, which can spread to deeper tissue such as joints or to the bloodstream.
The exact timeline between xylazine exposure and the development of these skin wounds is not known. But they typically seem to occur after repeated xylazine use, O'Neil and Kovach said.
"The wounds can be painful and disfiguring sometimes impacting people's ability to walk or use their upper extremities," the researchers said.
The doctors treated the man's wounds and by a six-month follow-up, they had healed well, according to the NEJM article. They also initiated buprenorphine therapy to treat the patient's opioid-use disorder. He subsequently began participating in an outpatient addiction program.
The exact prevalence of necrotic wounds among people who inject fentanyl adulterated with xylazine is not clear. But O'Neil and Kovach said they have been encountering people with xylazine-associated skin wounds on a weekly and sometimes even daily basis at their hospital.
"Due to the stigma of injection drug use, people may delay seeking medical care. Because of this, I suspect this problem is even more common in the community compared to what we have glimpsed in the hospital so far," the doctors said.
Outcomes for people with these wounds vary based on the site and size of the injury, the presence of infection and how quickly they present to the hospital for care.
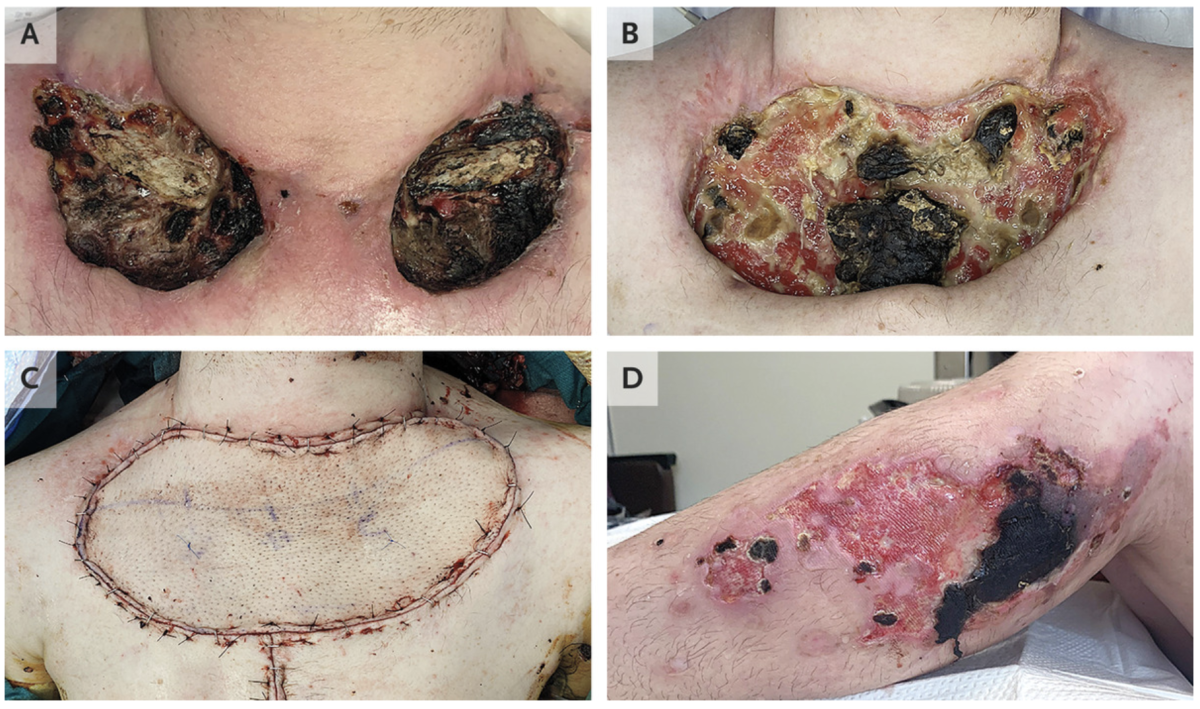
"In our experience, a small wound can heal with cessation of injection, cleaning of the wound and supportive wound care," the doctors said. "Even small wounds though can take several weeks to heal and can leave significant scars."
"A large, deep wound with superimposed infection may require a combination of antibiotics and surgery to remove dead tissue and close the wound with a skin graft or flap. We have also unfortunately observed a small number of people who have had such extensive tissue death and infection that they have undergone amputation of limbs."
O'Neil and Kovach said they had worked with several people who had successful healing of their wounds, including those with large, deep wounds requiring extensive surgeries.
"Successful treatment of this condition requires a team of specialists including plastic surgeons, dermatologists, infectious disease doctors, wound care specialists. And most importantly, addiction medicine specialists and social workers to support people through withdrawal, initiate substance use disorder treatment and connect them to resources for their ongoing care," they said.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Aristos is a Newsweek science reporter with the London, U.K., bureau. He reports on science and health topics, including; animal, ... Read more