Gun violence is scorching the United States, and the wound is increasingly visible. More than 11,000 Americans are killed in assaults involving guns annually, and at least 50,000 more are injured. Among people between the ages of 15 and 24, nine of every 100,000 lives end due to a gun homicide. About 65 of every 100,000 people in this age group are injured by gun assaults every year.
In the mid-1980s, public health experts began referring to youth violence as an epidemic because it was occurring in higher than expected numbers. Some experts took that notion further, insisting that youth violence isn't just like a disease—rather, it is a disease, an infectious pathogen akin to those responsible for AIDS and tuberculosis. Until now, that assertion has remained more poignant analogy than biting reality. But a new study provides the first evidence that gun violence behaves exactly like a blood-borne pathogen.
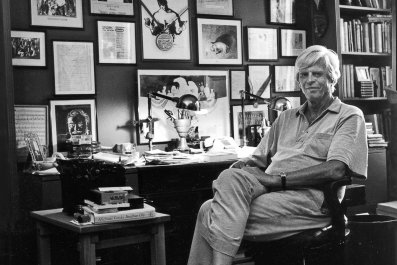
Andrew Papachristos, a Yale University sociologist who studies crime, knew that if gun violence was a disease, it should spread along a predictable path. And that path, he suspected, was social contagion, the same route taken by HIV and hepatitis C. Those pathogens travel by blood rather than bullets to reach new hosts, but outbreaks usually occur among networks of people who know each other. Diseases that spread through social connections follow a different pattern from airborne colds or food-borne illnesses, in which contagion among strangers is more common. Papachristos postulated that subjecting gun violence to a traditional epidemiologic study would reveal whether it indeed behaves like a blood-borne pathogen.
To conduct his study, Papachristos and colleagues at Harvard University turned to Chicago, which had more than 4,300 victims of gun violence in 2016. Combing the records of the more than 1.2 million arrests made in Chicago between 2006 and 2014, the investigators identified people who knew each other by focusing on co-offenders; that is, people arrested together for the same crime. They then homed in on co-offenders who'd been shot at some point in their lives, whether fatally or not. If gun violence spreads like a pathogen, they reasoned, then becoming a gunshot victim is akin to becoming contagiously infected: Once you "have" gun violence disease, you're probably going to give it to someone else.
The largest social network identified among the arrests included 138,163 people. That network accounted for more than 11,000 shootings affecting 9,773 people, whether as victim, perpetrator or both.
Having identified a network of gun violence, the researchers used a mathematical model to examine whether the spread adhered to known patterns of social contagion. Ben Green, who studies applied mathematics at Harvard, melded contagious-disease models with those tracking how information moves across social networks. The model assumed that closeness mattered—"You're more likely to influence a friend than a friend of a friend," says Green—and that exposure risk, meaning a gun violence victim infecting someone else, diminished over time.
The approach, says Myron Cohen, who directs the Institute for Global Health and Infectious Diseases at the University of North Carolina and was not involved with the study, mirrors exactly how epidemiologists scrutinize new physical diseases, especially in the absence of blood samples containing the pathogen. "The tools that they used are the tools that would be used in an outbreak investigation," says Cohen.
According to the results, published in January in JAMA Internal Medicine, 63 percent of gun violence cases were due to social contagion. As Green explains, this rate indicates that shooting victims were "exposed to gun violence by social contagion more than by any other factor." In other words, shooter and victim could be connected by tracing their social network (though they may not have known each other). The model revealed gunshot episodes proliferating through a cascade of people who knew each other—one victim exposes two friends, who become victims and then expose their friends. "The gun violence epidemic is even more epidemic-like than we've thought," says Papachristos.
The Chicago shootings included in the study occurred, on average, every 85 days, lending further support to the notion of gun violence as an infectious disease. Those 85 days suggest an incubation period, the time between a host becoming infected and a symptom appearing. Repeat gunshot events often occur within hours, says Gary Slutkin, infectious disease physician at the University of Illinois and adviser to the World Health Organization, who was among the first public health experts to see violence as a pathogen. But the short time frame in which people moved from being a friend of a new victim to a victim themselves—just a few months—was surprising. "That's an important finding," says Slutkin.
Although age, race, gender and gang membership are accounted for in the study, the researchers did not have data on education level, employment status and substance abuse, factors that "may put you at greater risk or inoculate you," says Papachristos. But even with these limitations, Cohen emphasizes that the study is important because it showed violence behaves "much like a disease."
Slutkin acknowledges the obvious difference between violence and viral or bacterial diseases: "There is not an infectious particle," he says. But he believes violence is infectious, entering a host not through the respiratory or circulatory systems but through the brain.
Slutkin founded Cure Violence, a nonprofit organization that addresses violence by intervening at points of contagion, such as immediately following a shooting, to quell the rage that fuels retaliation. But the notion of violence as an infectious disease has not been embraced the general public. He believes this study could bring wider acceptance of the infectious disease theory and an accompanying adoption of new approaches to addressing gun violence. Cure Violence focuses on intervening at points of risk, such as counseling victims and their closest friends and family immediately following a shooting event. Papachristos envisions a government-supported rapid response trauma specialists that would be dispatched across social networks to halt the spread.
Papachristos has replicated the model in seven other U.S. cities, and that work will be published soon. His next studies will examine the influence of other contacts in an individual's network—child welfare agencies, mental health counselors and the court system, among others—on the spread of gun violence and traits, such as resilience, that protect people in at-risk networks who don't get shot.
He hopes the present study will transform how we view perpetrators of gun violence: not just as criminals but as sufferers of a potentially fatal disease. That understanding, says Papachristos, clarifies the need for preventive and treatment measures beyond what the criminal justice system can offer. "This person is a victim," he says, "we need to save their life."