I am a millennial, which means that along with my deft technology skills and love for social media, I am also a member of the first generation to have never lived in an HIV-free world since the illness was first diagnosed in humans. The fact that 1.5 million people die from AIDS-related illnesses every year has been a part of my reality since birth.
One could even say millennials and AIDS have grown up together: As doctors first pulled us from our mothers' wombs, they were also identifying the human immunodeficiency virus as the newest viral threat to the human race. When we learned to walk, scientists learned they could beat back the virus's devastation on the human body with the discontinued cancer drug azidothymidine, better known as AZT. Later, as we were perfecting our ABCs and learning to count, pharmaceutical companies succeeded in perfecting the ideal AIDS "drug cocktail." It was no cure, but it extended and greatly improved the lives of patients suffering from the acquired human immunodeficiency syndrome.
The illness was transformed from a near-certain death sentence in the 1980s to a completely treatable condition by the 2000s. By 2010, great efforts had been made to remove much of the stigma that surrounds the virus and those it infects. Still, despite these advances, the cure for the virus remains elusive. But that might be because scientists have been looking for it in the wrong places.
The Berlin Patient
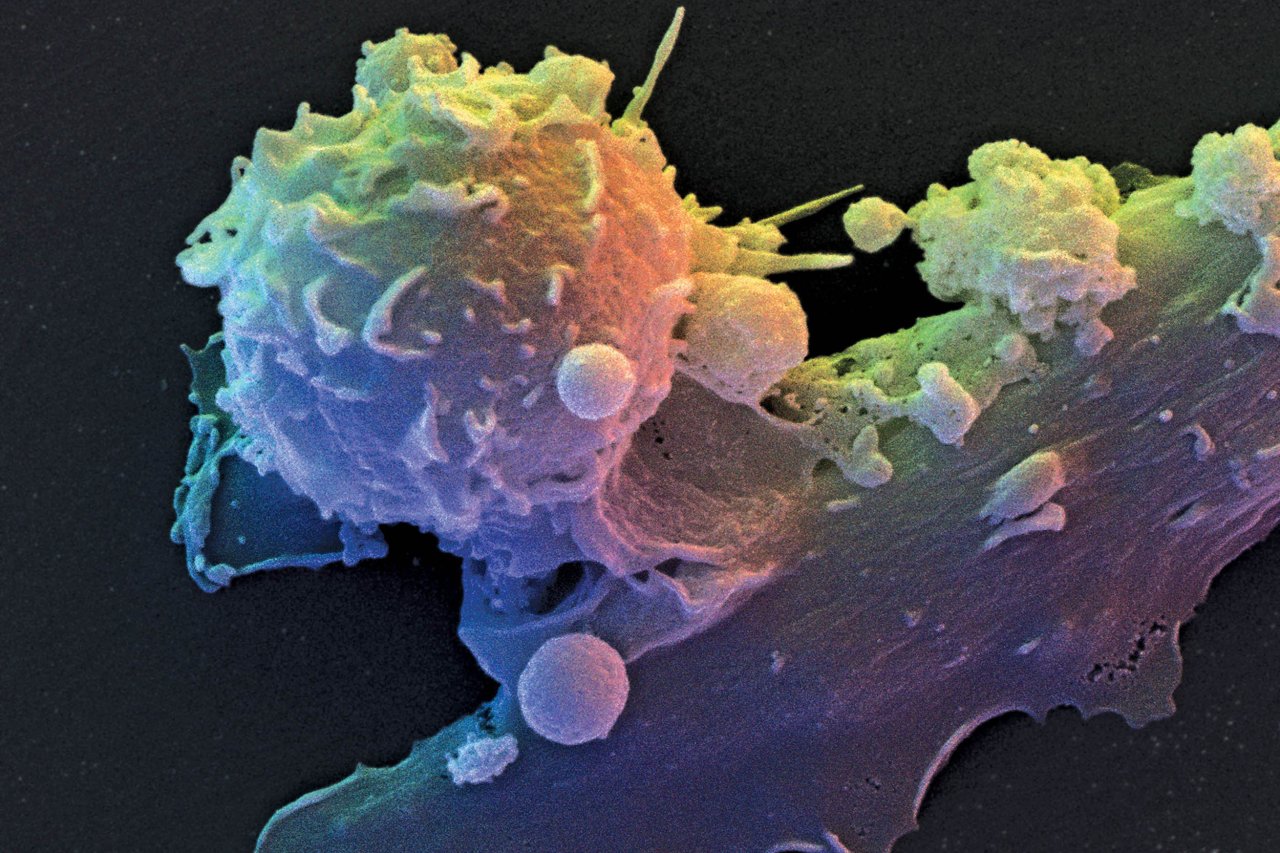
When HIV enters the body, it targets T lymphocyte cells (T cells) in the immune system. As these vital immune system cells are destroyed, the body is left with depleting defenses. If the virus progresses far enough, the patient will develop AIDS and become more susceptible to an array of pathogens—bacteria, fungi, parasites and other viruses—that a healthy adult body would fight off easily. AIDS patients are also more likely to develop cancer, and live with systemic symptoms of infection (regular fevers, weakness and weight loss, for example). But for every 100 people infected with HIV, one will show nearly no symptoms. These rare individuals are called "elite controllers" and are born this way due to a unique genetic mutation.
Except, in 2007, science managed to create one. That year, Timothy Brown, better known as "the Berlin Patient," become the first person to be cured of HIV by being turned into an elite controller.
In 1995, Brown's life forever changed when he learned he had tested positive for HIV. With the help of his doctors, he was able to control the virus using the relatively new treatment options, until 2006, when his health took another unexpected turn. Doctors informed Brown he had acute myelogenous leukemia, a form of bone cancer. His newest diagnosis was completely unrelated to his HIV status, but if nothing was done, the cancer would surely and swiftly kill him. Brown needed a bone marrow transplant, and in an ingenious move, his hematologist, Dr. Gero Hütter, decided that, rather than using marrow from a donor who simply matched Brown, he would take it one step further and use matching marrow from a known elite controller.
On February 7, 2007, Brown underwent the first of its kind procedure, and HIV history was forever changed. By 2009, tests revealed he was not only cured of cancer but also nearly HIV-free. His body contained only small traces of the virus, not enough for it to replicate or spread in any meaningful way
Doctors are still not entirely sure why Brown was able to develop immunity. Although the same procedure has been repeated on other patients, it failed to produce the same results. Seven years on, Brown remains the only patient to have ever become virtually HIV-free and stay that way.
Virus-Creating Factory
In the past, scientist sought out a cure by killing either the virus or the virus-infected cells. Both of these strategies have failed repeatedly, and will most likely continue to do so: Although antivirals can keep viral numbers down to undetectable levels, there seems to be no way to completely eradicate a virus from the human body.
But after Brown's miracle story spread, one team of scientists—including Nobel laureate David Baltimore and Hütter, the Berlin Patient's doctor—formed a company, Calimmune, to investigate a new approach. Rather than working to completely rid patients' bodies of HIV, they would try to replicate the experience of the elite controllers—and the Berlin Patient—who continue to have small amounts of the virus in their bodies but experience none of the health consequences, and don't need any of the medications used by other patients trying to control their HIV infection. If they succeeded, they'd have the first true "functional cure" for HIV.
"It's not the virus but how the host controls it that we need to be able to mimic," says Dr. Magdalena Sobieszczyk, a researcher with the HIV/AIDS Research Program at Columbia University Medical Center in New York.
It's all about the T cell. In order to enter a T lymphocyte cell, HIV must pass through a gene receptor referred to as CCR5. Think of CCR5 as the "doorway" to the cell. Once inside the T cell, the virus takes over and turns it into a virus-creating factory. A patient is considered to be stricken with AIDS when the viral "load" reaches a certain threshold.
In the case of elite controllers, the CCR5 gene receptor is mutated in such a way that the virus is unable to latch onto and enter the T cells. This means the virus is unable to replicate—and its numbers will remain so low that they are nearly undetectable by doctors.
Calimmune's researchers have used stem cell technology to create T cells lacking the CCR5 gene receptor, thus making them resistant to HIV. These manually mutated cells are then reintroduced into the patient's body via an outpatient transplant procedure that is more effective and safer than a standard bone marrow transplant. The latter, says Dr. Scott Hammer, a scientist at the HIV/AIDS research program at New York's Columbia University Medical Center, is too "toxic" of a procedure to be considered as a general treatment for HIV.
The transplant "gives them a population of cells that are not infected," says Baltimore. These uninfected cells could then either control the virus numbers in HIV-positive individuals or prevent infection in those without it. In other words, the transplant has the potential to be both cure and vaccine. Calimmune has announced it is about to move on to the second half of its Phase 1 human trial, and will soon implant four new patients with its genetically modified stem cells.
Scientists from Harvard have recently succeeded in artificially creating this same CCR5 gene mutation using the relatively new CRISPR gene-editing technology. CRISPR—short for "clustered regularly interspaced short palindromic repeats"—is a mechanism that allows scientists to precisely target and then edit any genes.
Chad Cowan, a researcher involved in the project, says that using CRISPR to edit the HIV patient's own cells in a petri dish and then reintroducing them back into the patient "would provide lifelong immunity or a cure for HIV." This procedure, he says, would "in essence replicate what is happening in elite controllers," and may also be able to reduce the patient's risk of transferring the virus.
To date, the Harvard gene-editing process has been conducted only in petri dishes; animal trials are the next step. Once the procedure has been shown to work in mice, the team would apply to the Food and Drug Administration to launch a Phase 1 human trial to test it for safety.
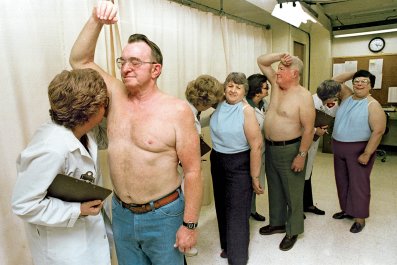
If it works, there's a chance that anyone diagnosed with HIV will be able to join the rarified 1 percent. Nathaniel Smith, who was diagnosed in 1989, hopes the treatment is perfected before it's too late for him. "I lived in a time when there was no hope, there was no treatment," he says. "People were told to get their affairs together because they have two years left to live."
Smith says that millennials diagnosed with HIV today have much more reason for optimism than any previous generation. But he's got a positive attitude about his future, too. "With all the advancements, I'm hopeful. Anything is possible."