Under cover of darkness, a few burial workers pried open the hospital morgue's steel doors and stole three corpses. They carried the bodies to the hospital's front gates and tossed them beside the road that bisects downtown Kenema, the third largest city in Sierra Leone.
As the sun rose, a crowd gathered around the bodies. No one admitted to dumping them, but members of the hospital's burial team, the 23 men tasked with carrying and cleaning Ebola-infected corpses, told local journalists the cadavers were a form of protest. The workers had not received the $115 weekly in "hazard pay" they had been promised for nearly two months by supervisors, the government and donors. And they were not alone. All over the country, hundreds—if not thousands—of doctors, nurses, hospital cleaners, lab technicians and burial workers had been unpaid or underpaid, and many still are.
That silent protest took place on November 25, 2014, while hospitals throughout the country were collapsing under the weight of the deadliest Ebola outbreak in history. The men and women on the front lines, risking their lives to save the dying and protect the healthy from infection, had begun to feel duped. Millions of dollars flowed into Sierra Leone from all over the world to help tackle the crisis, but the workers' pleas to be paid were ignored.
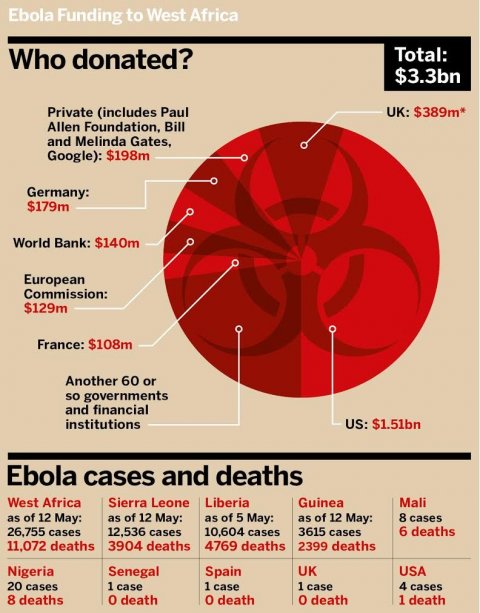
The lack of wages was not simply a matter of corrupt officials stealing donor money. Instead, there appear to be two additional problems: First, Sierra Leone's national health system has been so underfunded for so long that it was a monumental challenge to document all the country's care workers and set up distribution channels to pay them. Second, relatively little money was reserved for local front-line staff within the national health system—less than 2 percent of $3.3 billion in donations to fight Ebola in West Africa was earmarked for them. The vast majority of the money, donated from taxpayers of the United States, the United Kingdom and two dozen other countries, went directly to Western agencies, more than 100 nongovernmental organizations (NGOs) and the United Nations.
While some health workers staged strikes over their mistreatment, many suppressed their anger and pressed on with their jobs. They did not want to risk their prospects of eventual pay—or the loss of employment. Indeed, the entire burial team at Kenema Government Hospital was fired after the corpse demonstration.
The day the bodies were dumped, nurse Elizabeth Kabba ignored the crowd gathered at the hospital gates, slid into her protective uniform and entered a makeshift structure of plywood and tarp, with the words "High-Risk Area" scrawled across the doorway in permanent marker. She had worked as a nurse in the Ebola ward since May, when Dr. Sheik Umar Khan, West Africa's leading virologist, first opened its doors. Khan had recruited her, plus a dozen other nurses from the general hospital—one of the largest in the country. Back then, no one could have predicted how horrific the outbreak would be. Ebola would kill Khan and 36 other health workers at Kenema Hospital. Across the three affected countries in West Africa, 507 health workers had died of the disease as of May 6, according to the World Health Organization (WHO).

When I visited Kenema Hospital in February, graffiti on one wall of the Ebola isolation area read: "Please pay us." By then, Kabba had cared for more than 420 Ebola patients and lost several friends. She also had not received most of the $92 weekly allowances she'd been promised since September. Nurses around the country were in similar positions. "We hear about money pouring in, but it is not getting to us," Kabba said. "People are eating the money, people who do not come here. We are pleading nationwide. We have sacrificed our lives."
THE WALKING DEAD
When Ebola crept across Guinea's porous border and into eastern Sierra Leone, it was the national health workers who responded. By July 2014, Khan's Ebola ward at Kenema Hospital had more than 100 patients. With a nearly 70 percent chance of a swift, painful death, people perished in their beds and on the floor; nurses climbed over corpses to reach other patients crying out for help. Invalids died while nurses rehydrated them, and cleaners wiped infectious fluids from their bodies. "I'd stay by their beds and pray for their lives to help them cope," said Miriam Conteh, one of the nurses in Kenema. "I'd lie and tell them I was once an Ebola patient, and that I survived and they can too."
On July 29, Ebola killed Khan. His death reverberated throughout West Africa, but it was felt most strongly at Kenema Hospital. "He was the captain of the ship, and when he died, everything changed," said James Massally, the hospital's lab director. "The attitude of workers, nurses, technicians—everyone was terrified."
To keep public clinics and hospitals staffed, the government promised hazard pay to health workers. Prior to the outbreak, nurses who were lucky enough to find paying jobs in the national health system usually earned about $130 per month—less than motorcycle taxi drivers. Many who weren't yet on payroll worked for free until a job opened. To get by, nurses sold goods on the side or charged patients extra. So when the bonuses were announced, thousands of nurses and other staff volunteered. Those treating Ebola patients directly were to get about $115 per week on top of their meager salaries; those in Ebola triage units, $92; and nurses in general wards, $46.
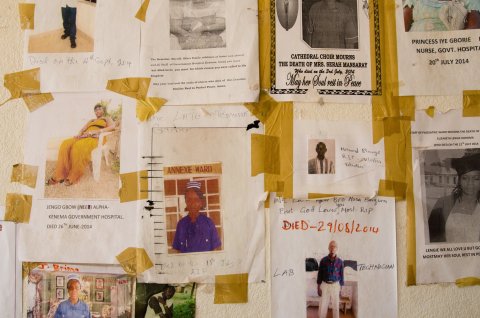
It soon became clear, however, that Sierra Leone could not afford to pay the staff needed to hold back the rising tide of Ebola. At Kenema Hospital, WHO contributed to hazard pay funds for a couple of weeks and recruited a handful of international health workers to help. Nahid Bhadelia, an infectious disease physician from Boston University, arrived in August to find fliers commemorating dead nurses and lab technicians hung on the walls—and a facility without rubber gloves, plastic Tyvek suits and other necessary safety equipment. "So you're not getting paid, your friends are dying and you have nothing to protect yourself. We couldn't get anything into the country because commercial shippers stopped flying," she said. "At one point, we created aprons out of tarps."

In August, after nearly 1,000 people had died of Ebola, WHO declared a world health emergency and the process of organizing and funding an international campaign to fight the contagion began. The world's largest donors searched for organizations to deliver their aid. But that took time, because few NGOs specialized in emergency clinical care, and the rare ones that did, like Doctors Without Borders, were stretched to capacity. In the meantime, the death toll in the three hard-hit countries—Sierra Leone, Guinea and Liberia—tripled. By October 1, it included 3,330 people.
In November, the World Bank, along with the African Development Bank, offered to cover the rising cost of hazard pay. Almost immediately, the World Bank noticed signs of corruption. When it looked at the lists of front-line staff created by officials in Sierra Leone's Ministry of Health, it discovered "ghost workers"—aliases, family members and mistakes in enumeration. "The lists were bloated, and it pointed to some malfeasance," said Sheriff Mahmud Ismail, a communications officer with the World Bank in Sierra Leone.
In response, the World Bank suggested using an e-pay system in which health workers would receive money directly to their bank accounts or via text messages instructing them to go to pay stations to pick up cash. With e-payments, government officials could not steal the money. According to the World Bank, the U.N. Development Program (UNDP) was brought on to manage the hazard pay database and coordinate the payment system: Hospital supervisors passed new lists of front-line staff to coordinators in each district, who examined and signed the papers before sending them to Freetown. There, a small team of staff from both the U.N. and the National Ebola Response Center (NERC, Sierra Leone government officials) corresponded with a U.S.-based accounting firm, BDO, to be sure the appropriate signatures were in place. If it all looked correct, the World Bank had BDO release the funds.
This small team in Freetown was responsible for overseeing $23.7 million of hazard payments to a fluctuating workforce of about 23,000 nurses, lab technicians and support staff throughout Sierra Leone. It was a monumental challenge in a country with a cash economy, no digital human resources database, a dearth of accountants and a history of corruption.
So it is not surprising that from November until today, complaints of missing hazard pay persist. "Since the beginning [of the Ebola response], the most consistent problem has been the failure to pay risk allowances," said Oliver Johnson, the director of King's Sierra Leone Partnership. "It's inexcusable with all of this money lying around that nobody has invested in a big team that can sort it out."
'I AM DELETED'
When I met Faith Sisay, she spoke bitterly of promises to support the "angels." She had worked at the Ebola ward at Kenema Hospital since the previous June, and continued to do so after she realized she was pregnant in August. In her early 20s, Sisay had just completed her nursing degree and needed the weekly stipends, as well as the pledge of post-Ebola employment made by Sierra Leone's president, Ernest Bai Koroma. Once her womb perceptibly swelled, the head nurses asked her to remain outside the ward, to prepare medications and fetch supplies. Initially, she received her hazard allowance, but then paydays in October, November, December, January and February came and went, and Sisay didn't receive a cent.
Beads of sweat collected on her nose as we chatted on her back porch; Sisay's huge belly seemed to burst out of her tiny frame. When she complained to her supervisors about missing hazard pay, they told her to be patient. But nothing changed. "They don't even know about Faith," she said. "I am deleted."
Back at Kenema Hospital, I watched young men from the former burial team don their protective gear and load a corpse into the back of a truck. Ebola was no longer ravaging the region, but people continued to die of various causes, and their corpses needed to be handled safely. Although the workers had been fired after the corpse-dumping demonstration in November, they continued to work for occasional tips. One of the men, Abdul Sam, invited me to see where he'd lived during the peak of the outbreak in Kenema. A thin white sheet covered a corpse in a corner, near a rusted steel cabinet. At the opposite end was a narrow, sectioned-off corridor, where Sam said he'd rested. By sleeping beside a pile of bodies, he was able to prepare Ebola victims around the clock. Then he was discarded. "No pay!" he gasped in a voice that climbed toward a falsetto, palms raised to the sky.
Massally supported Sam and a few others with his own money after they were laid off in November. He had worked with the U.N. in East Timor in 1999, he said, and has a sense of how much money flows through the hands of the people who tackle a crisis via laptop. "I feel pathetic for the local staff. They do everything, but the returns go to the internationals, who do not go into the red zone," he said. "Some do, but it's a relative few."
On the outskirts of Kenema is an Ebola treatment center operated by the International Federation of Red Cross and Red Crescent Societies, which opened after the worst of the outbreak had passed through the district. By November, patients diagnosed with Ebola at Kenema Hospital were transferred there for care. When I visited in February, there were no patients at the unit. Two dozen local nurses sat in the shade of a tent, waiting for a training session on hand-washing. They say their salaries and hazard payments were consistent, reliably processed by the NGO.
Just down the road, at Kenema's public hospital, I met Miriam Conteh, in faded maroon scrubs darkened with sweat. She had been at the hospital's Ebola ward until 3 a.m. the night before with a patient she now suspected suffered from Lassa fever, a viral disease that, like Ebola, is characterized by bleeding. Conteh told me she could help me document who worked in the Ebola unit, and deserved hazard pay, but only in secret because nurses were warned not to complain to outsiders. A nurse who had told a local journalist about his pay problems had been transferred to another district. Nurses around the country echoed the concern. For these reasons, the names and some distinguishing features of the health care workers have been changed in this article.
Conteh arrived at my guesthouse a few days later, carrying a backpack heavy with documents. The loose papers formed a rough diary. A page from July 23 read: "29 confirmed Ebola patients, 3 in critical condition, 1 lactating mother, 6 orphans, 8 in need of psychosocial support, 2 dead, 41 nurses on duty for all shifts." Papers from the laboratory showed that technicians in Kenema had tested 3,083 patients and 742 corpses for Ebola from May through November. Log books listed staff in the Ebola ward over time. For every name, Conteh described the person: He was a diligent cleaner, she was a fat nurse, and so on. Conteh said several had not received hazard pay for several months, and many of the others—including her—had been paid only half.
I converted the staff lists to an Excel file and emailed it to the UNDP in Sierra Leone. Sudipto Mukerjee, the UNDP country director, met me in his office in Freetown. Just before, someone on his team searched in their system for some of the nurses on my list and replied with a subset of names they found. Mukerjee said everyone on that subset list had received their weekly pay (but later said to verify that with government officials at NERC). I told him about nurses not on the U.N.'s list who had not been paid, and I said that those who were on it had insisted they had received half the promised amount. "November payments have been paid, as far as I am concerned," he told me. "And if they say they aren't [paid], they should lodge this complaint through a proper system and not through you." I replied that they are threatened if they complain. "If you have a situation where people are being threatened, they should report it to anti-corruption [agencies]," Mukerjee countered. "They should report it to the police, to the traditional chief: There are so many means of getting your voice heard."
When I left his office, I called a senior nurse in Kenema to ask if—as Mukerjee suggested—their problems ceased in November. She sounded shocked. "They should see what we went through on the front line while these people sat in the AC, in their own vehicles, while we were sweating," she said. I decided not to tell her that internationally recruited U.N. staff earn $1,600 in danger pay every month on top of their significant annual salaries; country directors in Sierra Leone, for example, take home $153,825 to $187,904 per year.

In a final attempt at clarification, I met with Awul Wurie, a manager from the NERC on the pay team, at the U.N. Special Court. I asked him for specifics on who had received what and when. "You have the nerve to ask me for private information?" he said. "I'm done with this. We're done."
In a follow-up email, Mukerjee clarified that UNDP is assisting the government in ensuring that people are paid appropriately and on time, but they are not responsible for names missing from lists or any misclassifications. A 2015 report from the U.N. states that the UNDP is supporting the issuance of hazard pay to Ebola response workers in Sierra Leone. According to the report, all the registered workers have been paid. The head of the District Ebola Response Center in Kenema, Abdul Wahab, reiterated this claim, just after I spoke with several unpaid staff. In an email, a World Bank spokesperson wrote: "The majority of workers who have earned hazard pay are receiving it." Perhaps, she suggested later on the phone, the nurses misspoke.
This lack of accountability is a common characteristic of U.N. agencies, said Rupert Simons, the CEO of Publish What You Fund, a London-based organization that pushes for aid transparency. "U.N. agencies will say the local government is in charge, but they have responsibilities—in this case for making sure that the World Bank's funds for hazard pay get out there. So they need to be held accountable to the World Bank, and the World Bank is accountable to its board of governance, who are governments, i.e., you, the taxpayers. There is a very long chain of accountability here, but taxpayers are at the root of this." That's true for the World Bank, which is essentially owned by the governments of 188 member countries, the U.N., which has 193 member countries, and for each bilateral donor—such as the U.S. and the U.K.—that acts on behalf of its citizens and with its citizens' money.
To their credit, the World Bank and the African Development Bank, with the U.N.'s support, offered money to front-line workers in Sierra Leone's health system. The world's largest donors to the Ebola response—the U.S. with $1.5 billion and the U.K. with $389 million, thus far—mostly gave their funds to NGOs, Western and U.N. agencies. After each organization absorbed a chunk, the remains trickled down to the local and international staff working with patients (generally outside the national health system) and to communities affected by Ebola. Some of the expenditures were undoubtedly effective, and some were wasteful, but it's difficult to discern between the two because budgets are opaque.
For example, the U.S. gave $423 million of taxpayers' Ebola response money to the U.S. Centers for Disease Control and Prevention. The agency has run more than 12,000 diagnostic tests for Ebola, monitored more than 150,000 travelers exiting West Africa, kept a large team of press officers rotating through Sierra Leone and more. But when I asked these officers how much money went to each of these services, I didn't get numbers. Several NGOs directed my budgetary queries to the donors that gave them money. Donors linked to websites with incomplete information. The totals don't match up. Grants for many thousands of dollars are described vaguely as "health," "Ebola support" and "Ebola response."
After the 2010 Haiti earthquake, an economist at the Center for Global Development in Washington, D.C., Vijaya Ramachandran, attempted to track $6 billion in taxpayer donations and concluded it could not be done. "A question worth asking is why we rely on this model of going through expensive NGOs rather than relying on domestic systems," Ramachandran said. "Corruption is often used as an excuse to not build up the local system."

SALARIES ARE NOT SEXY
What is obvious to anyone in Sierra Leone is that much of the aid money donated before and during the Ebola crisis has returned to people from donor countries. Dozens of international NGOs have settled in Sierra Leone since the "blood diamond" civil war ended in 2002. Their overhead is relatively high because international staff expect living wages, Internet, health insurance and flushing toilets. During the Ebola outbreak, it was even higher because they required expensive security measures, such as private four-wheel-drive vehicles and hotels with ATMs and surveillance cameras. The U.S. Agency for International Development booked every standard room in the Radisson Blu—which typically cost $270 per night—for six months.
Emergency responses aren't about finding the cheapest option, I was told; they're about speed. Still, expensive doesn't equal effective. The situation with stand-alone Ebola treatment centers illustrates that point: Just 28 Ebola patients have been treated at 11 Ebola centers in Liberia that cost the U.S. hundreds of millions of dollars, according to a New York Times investigation.
What's more, stand-alone treatment centers have already begun to pull up stakes as the outbreak ends, while the public hospitals stay busted. This model of providing assistance outside of the health system has been the norm for aid to Sierra Leone for over a decade. It creates a cycle of dependence: Even when the aid saves lives, the infrastructure required to deliver services in-house is not built, and as a result, the country remains ever reliant. Sierra Leone's health system is one of the world's worst. According to the WHO, the minimum threshold of doctors, nurses and midwives required for access to basic care is 22.8 professionals per 10,000 people. The ratio in the U.S. is 100 per 10,000. Sierra Leone's is 5.
At Sierra Leone's biggest referral hospital, Connaught, in Freetown, mobs of patients lingered at the entrance in February. I spoke with the head nurse of the overrun emergency ward in his office—in a supply closet. He was missing hazard payments, frustrated with his low salary and depressed with the lack of services he could offer patients. If someone arrived in the throes of an epileptic seizure, he'd have to ask them to go to a pharmacy and buy a needle and catheter, because the hospital didn't have any.
Health professionals in Sierra Leone often seek out better-paying jobs with NGOs, or in other countries if they're able. In December, the British government held a hearing to review the U.K.'s Ebola expenditures, handled by the Department for International Development. Stephen Phillips, a conservative member of Parliament, asked why Sierra Leone's national health system was anemic after 15 years of British aid. "When this outbreak comes along, the British taxpayer finds that there are only 120 doctors in the entirety of Sierra Leone," he said. "Isn't the magic bullet for DFID and the international community to supplement terms and conditions in a way that encourages medically trained staff to remain in their home countries?" Mark Lowcock, DFID's permanent secretary, replied that it had been tried, and it failed.
The philanthropist Bill Gates, the U.N. and the WHO have released recommendations on how to strengthen weak health systems so that the world will be better prepared for future outbreaks. Their advice includes equipment, isolation units, affordable health care, workshops for nurses, surveillance systems, technological solutions and pharmaceutical products. But none that I've found mention pay.
A common dismissal of the idea of donating directly to local nurses and other health workers is that underwriting salaries is unsustainable. Another explanation is that it discourages African governments from paying their civil workers. A more jaded hypothesis is that salaries are not sexy. Do-gooders prefer tangible displays of generosity—air-conditioned biohazard suits, iPads for data entry and other gifts that look good in video montages. Another possibility is that those calling the shots have little incentive to change a system of aid that is attractive to those on the giving end. As a Sierra Leonean economist told me, on condition of anonymity for fear of jeopardizing his ailing country's relationship with donors, "It's in their interest to make us look bad so that they can hold the budget. The NGO industry is an industry."
Whatever the reason, the fragile health system that permitted Ebola to become an international disaster is now in even worse shape. While Ebola raged, people sick from pregnancy complications, diabetes, measles and myriad other maladies stayed away from hospitals for fear of the bloody disease. Now they're returning to find a staff depleted from health worker deaths and deflated from the horrors they witnessed. Infectious disease scientists guarantee this will not be the last outbreak in our lifetime. The head of Kenema Hospital, District Medical Officer Mohamed Vandi, has grown weary of the buzz about "health system strengthening" touted by global health leaders. "If I could not get support when the virus was here," he said, "how could we get it when the virus is gone?"
Perhaps with more time, manpower and pressure to do the job well, the U.N., the World Bank and Sierra Leone's government might have sorted out e-payments. There were hints of improvement after I left the country. In March and April, the pay team returned to Kenema to investigate. On April 9, Kabba called me to say she had been paid in full for February, although she still lacked half of her hazard pay from the months prior. She suggested I call Faith Sisay, who had just given birth to a "bouncing baby boy." On the phone, Sisay thanked God for her healthy child, but added that she had received no payments and had lost hope in the system. "When the next disease comes, it will be difficult to get nurses," she said. "How will you do it?"
Support for this story was provided by a travel grant from the Pulitzer Center on Crisis Reporting and investigative funds from Tiny Spark.