The outbreak of Zika virus in Brazil in 2015, which brought the pathogen to widespread attention, came as a shock. The virus, discovered among caged monkeys in the Zika Forest of Uganda in 1947, had been presumed to be harmless to humans. Three cases were reported in 1953 in Nigeria, but no other incidents followed for more than 50 years. A 1971 study showed the virus could kill newborn mice, but that still didn't raise concerns. "The entire world ignored this virus," says virologist Richard Zhao of the University of Maryland School of Medicine. A 2007 outbreak in Yap, an island in the Federated States of Micronesia, was followed by others in French Polynesia in 2013 and 2014, followed by Brazil.
But the Brazil outbreak was what made everyone take notice. It wasn't just emergence of a new human pathogen in a large, highly populated country that was disconcerting. It was also the birth defects. Mothers infected by Zika were giving birth to babies with abnormally small heads. Known as microcephaly, this brain malformation is linked to developmental delays, seizures and other serious neurologic problems.
Initially, whether the virus was causing the defects or not was unclear. When the World Health Organization declared clusters of microcephaly and Guillain-Barré syndrome to be a public health emergency in February 2016, the clusters were not conclusively tied to Zika. Soon enough, though, researchers at Florida State University and Johns Hopkins University showed that the pathogen was definitely the cause.
The infant microcephaly was "an incredible surprise," says Mark Challberg, who oversees flavivirus research funded by the National Institutes of Health. The flavivirus family includes Zika, as well as yellow fever, dengue, West Nile and hepatitis C, none of which cause congenital defects in babies born to infected mothers.
By April 2016—less than a year later—the pathogen had spread, by mosquitoes and sexual transmission, to more than 60 countries and territories, including the United States. Brazil confirmed more than 1,000 cases of microcephaly and other central nervous system abnormalities directly tied to Zika, with another 4,000 under investigation. Thirteen countries had also reported incidents of Guillain-Barré syndrome, which causes a temporary paralysis, among infected adults.
According to current estimates, 1 to 13 percent of Zika infections during the first trimester lead to microcephaly. One study found 29 percent of infants born to Zika-infected mothers in Rio de Janeiro had some brain abnormality. No vaccine or treatment for the virus exists.

As he watched the epidemic unfold, Zhao was haunted by one question: How does Zika work? "We knew the virus as a whole causes damages," he says. "But how exactly the virus does that, we did not know." Years earlier, Zhao had made crucial strides in uncovering the inner workings of HIV. He was determined to do the same for Zika.
To understand how Zika harms fetal brains, Zhao needed to study its components one by one. And he needed a way to witness the damage each piece wrought. Fission yeast, he knew, would serve both purposes.
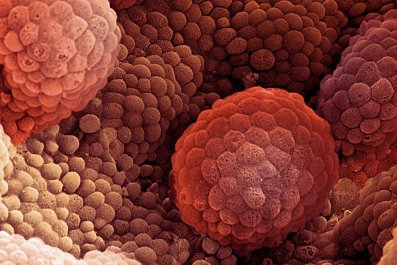
Fission yeast—Schizosaccharomyces pombe, in scientific terms—was first used to study cancer cells in the 1950s by Sir Paul Nurse, a British scientist who won a Nobel Prize in 2001. The yeast, which is used to make beer in Africa (pombe is Swahili for beer), is a single-celled organism that grows easily and has many properties similar to human cells. An estimated 50 genes implicated in human diseases are present in fission yeast DNA, and cell division in both life forms also involves several of the same genes. Zhao had already used fission yeast to study HIV and barley yellow dwarf virus, which attacks several grasses. By dismantling the Zika viral genome and observing the encoded proteins inside fission yeast, Zhao thought he would be able to spot the enemies in action.
Zika contains a single strand of RNA encoding 14 distinct proteins. As Zhao and his team exposed colonies of yeast cells to each protein, they noticed that seven of the proteins impaired yeast growth in one way or another.
The growth delays, cell deaths, warped shapes and other disruptions are all routes that could lead to microcephaly along with the other, less common neurologic problems caused by Zika, including congenital deafness, eye abnormalities and spina bifida.
That the seven proteins identified by Zhao are in fact responsible for these problems has yet to be proved. Stevens Rehen, who teaches biomedical science at the Federal University of Rio de Janeiro, points out that because the study used the 1947 strain of the virus, the findings may be irrelevant. Zika, like other RNA viruses, mutates rapidly, so the mechanisms by which it damages brain cells today may not have been present in earlier decades. Zhao says he decided to use the original strain so that even if the experiment revealed no harmful proteins, the results would provide a baseline comparison for subsequent research.
The new study, published in December in Proceedings of the National Academy of Sciences, could contribute to Zika treatment efforts. The yeast system can be used to screen for potential new drugs, says Jae Jung, a molecular biologist at the University of Southern California who recently identified two culprit Zika proteins using a different model. Jung cautions that the virus may not produce the harmful proteins at the same high quantities to which the yeast cells were exposed. Still, adding potential drugs to the Zika-yeast mix is a simple way to test whether they interfere with the cell killing. "Alive or dead is very easy to screen for," he says.
Challberg emphasizes that a Zika vaccine is a priority over treatment. But even if scientists create a successful inoculation—at least two are being tested—a medication could still be useful because some vaccines are given after an infection occurs. "If you can slow down the disease, that could give you more time to suppress the virus," says Hengli Tang, a collaborator on the work linking Zika to microcephaly. (He provided Zhao with Zika samples.) Next steps include studying the seven proteins in animal and human cells and examining more recent strains of the virus to see how they differ from the 1947 samples.
Even if studies like this don't lead to a treatment, Tang emphasizes that understanding the dangerous proteins is critical. In the U.S. alone, more than 4,600 cases of Zika have been reported, with more than 1,000 among pregnant women. "We don't know what will happen next," says Tang, "and what other viruses will emerge like this that we're just not prepared for."
And in the meantime, scientists like Zhao will continue preparing for the viral threats, such as Zika, that are already here.