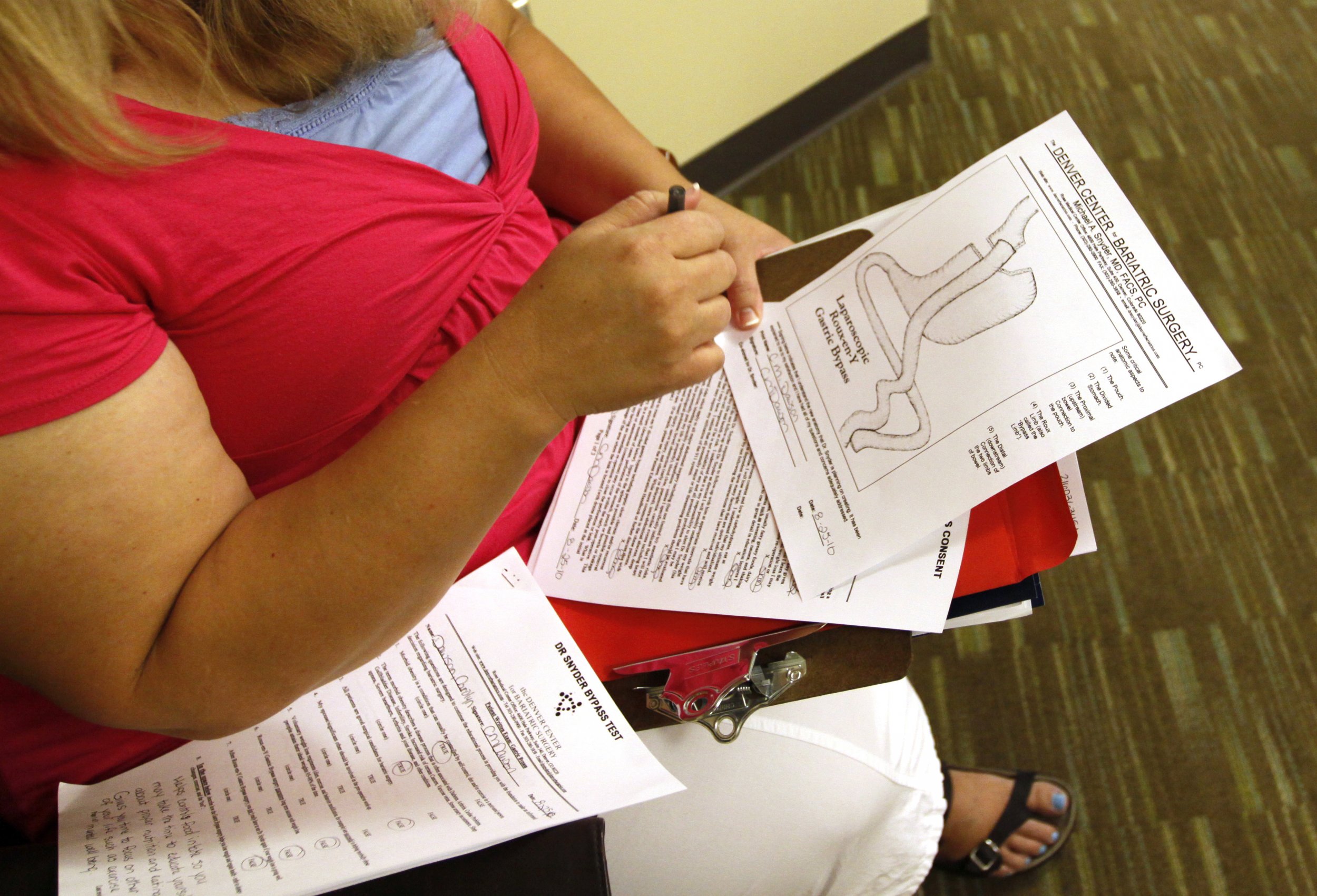
Bariatric surgery has been, quite literally, a lifesaver for countless people struggling with extreme or morbid obesity. As these procedures have become more sophisticated, safer and effective, doctors are more likely to use them as an intervention in clinical medicine.
But a new study, published in the July issue of JAMA Surgery, suggests weight loss surgery is happening far too late for patients to achieve the best results, which include a body mass index (BMI) below 30 and reversal of chronic obesity-related diseases such as diabetes. BMI is a measure of body fat based on a person's weight in relation to their height.
Bariatric surgery is an operation to reduce the size of a person's stomach in order to limit the amount of food he or she is able to consume in a single sitting, thereby making it easier for a person to lose weight. There are a number of ways physicians can accomplish this. A band applied to the stomach can make it smaller; a portion of the stomach can be surgically removed; or the small intestine can be rerouted to a small stomach pouch. But because all of these procedures are relatively new, when to offer it to patients with obesity has been a matter of debate, resulting in dangerous delays.
Researchers at the University of Michigan have taken a significant step toward clearing the air. They reviewed medical records of 9,173 patients who underwent weight loss surgery. Of that group, 36 percent had achieved a BMI of less than 30 a year after their surgery, the ideal score. But in analyzing the data, they found a clear indicator of meeting this goal was having a BMI below 40 to begin with. Comparatively, only 8.5 percent of patients with a BMI higher than 50 were able to reach a BMI of less than 30 a year after the surgery. In the study, the average preoperative BMI was 48. In other words, delaying bariatric surgery until further weight gain often defeated the point of the surgery.
"Bariatric surgery is often considered as the last resort for treatment of obesity when all other attempts have failed," says Oliver Varban, who directs the adult bariatric surgery program at the University of Michigan Health Systems and was lead author on the study. "Of course, they will lose a significant amount of weight and have some health benefits, so the idea here is not to restrict bariatric surgery to patients with really high BMIs, but instead to promote earlier referral and less restrictions among patients with lower BMIs."
He adds that the research suggests the typical approach—to wait until a patient's BMI is extremely high (above 50)—appears to make the surgery less effective. Delaying the procedure means the patient will have a harder time achieving weight loss that leads to a healthy BMI (below 30).
The U.S. Centers for Disease Control and Prevention and other public health authorities say a healthy BMI for adults is between 18.5 and 24.9. (An adult with a BMI between 25 and 29.9 is considered overweight, while someone with a BMI of 30 or above is classified as obese.) Severe, or morbid, obesity is classified as a BMI of 40 or higher.
And the benefits of surgery extended beyond reducing BMI. The researchers found patients who had weight loss surgery earlier were able to reduce or discontinue medications prescribed by doctors to manage conditions such as high cholesterol, diabetes and hypertension. "If bariatric surgery can cure diabetes, why limit this treatment to people with severe obesity?" says Varban.
The delay in bariatric surgery goes against the usual medical grain. Often physicians offer surgical interventions far earlier to their patients, says Verban. "This is why I found it so compelling that the average preoperative BMI was 48 in our study," he says. He theorizes that other factors affecting the referral process to surgeons or barriers placed by insurance companies could be responsible for the delay.
For example, he says, many insurance companies require six to 12 months of documented medically supervised weight loss. "However, if the patient has a BMI over 50, this requirement is waived," he points out. "Thus, in order to avoid this onerous requirement, patients and referring physicians may simply wait until their BMI is over 50 before deciding to pursue surgery."
Regardless of a preoperative BMI, bariatric surgery isn't enough to help a patient reach a healthy goal weight. "I can see how some would see surgery as a magic bullet, but the physiology of metabolism in the human body is really complicated with many layers of redundancy, all of which may differ from person to person," he says. Surgery is one more tool to change the body, "beyond what diet and exercise can do alone."
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Jessica Firger is a staff writer at Newsweek, where she covers all things health. She previously worked as a health editor ... Read more
To read how Newsweek uses AI as a newsroom tool, Click here.