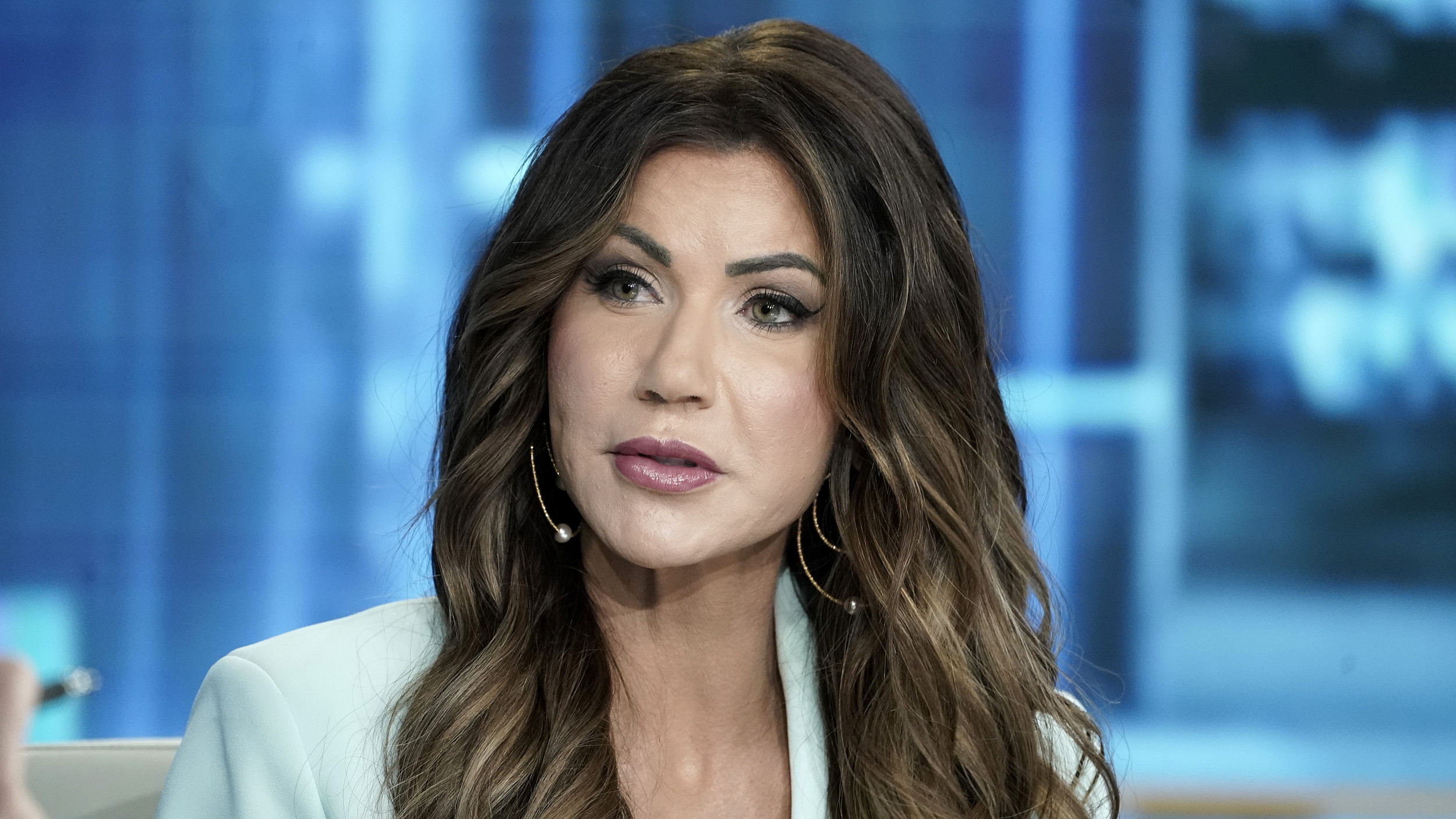
A Houston woman who had an allergic reaction to a COVID vaccine has encouraged others to get the shot.
Raana Bell, who has a history of allergic reactions, received her first dose of the Pfizer-BioNTech vaccine last Wednesday but ended up in an emergency room soon after, KHOU reported. She was released from hospital later that day after receiving treatment.
But despite her negative experience, Bell told KHOU: "I think the vaccine is imperative. I don't think it's a decision of should you get the vaccine or don't if you are able to do so."
Bell said she didn't want to scare people off receiving a COVID-19 vaccine but thinks there needs to be more transparency regarding the shots, particularly for people with a history of allergic reactions.
Bell is eligible to receive the vaccine as part of group 1B because she has an underlying medical condition.
"Knowing there was a vaccine coming was, to me, lifesaving. It really was," Bell said.
But within around 15 to 20 minutes of receiving her first dose of the Pfizer-BioNTech shot, Bell began feeling a burning sensation in her left arm and the left half of her body.
"My chest started feeling very tight. I know what this kind of reaction feels like from reactions I've had to other medications," Bell said.
Medical staff at Houston Methodist Hospital, where Bell received the shot, took her to the emergency room and treated her with medications, including steroids and breathing treatments.
Eventually her condition improved and she was allowed to leave that evening. While Bell said she feels much better, some side effects from her reaction have lingered.
Bell said she is now discussing with her doctor before she receives her second dose of the vaccine.
She encouraged people with a history of allergic reactions to consult with their physicians regarding the vaccine.
"Do you need to do, like, in my case, breathing treatments and steroids before? Have that discussion before you show up for your vaccine. It's a very simple discussion but could really save a lot of distress you may have," she said.
"I know we don't have a lot of control over where we get it, but we do have control of the conversations we have with our doctors and having a loved one there with you."
Severe, life threatening allergic reactions—known as anaphylaxis—are rare following vaccinations.
According to a Centers for Disease Control and Prevention (CDC) report published on January 15, the Vaccine Adverse Event Reporting System detected 21 cases of anaphylaxis after the administration of 1,893,360 Pfizer-BioNTech first doses in the period December 14-23.
This works out to around 11.1 cases per million doses—which, according to the limited data available—is very low and comparable to other vaccines, albeit higher than the rate at which these reactions occur following administration of the flu vaccine.
The CDC said 71 percent of these reactions occurred within 15 minutes of vaccination. Seventeen of the individuals had a documented history of allergies or allergic reactions. Of the 20 people with available follow-up information, all had recovered or been discharged home.
The CDC said COVID vaccines can only be given Emergency Use Authorization if the known and potential benefits outweigh the risks of the disease.
The agency has issued a list of guidelines for people who experience an allergic reaction after receiving a shot, or who have a history of allergic reactions.
The agency said anyone who has a severe allergic reaction—one in which the person needs to be treated with epinephrine/an EpiPen or requires hospitalization—after the first dose of the currently available vaccines should not get the second dose.
This recommendation also applies to people who experience non-severe allergic reactions within four hours of receiving the first dose.
In addition, if you have had any kind of allergic reaction to any ingredient in the mRNA COVID-19 vaccines, the CDC recommends that you should not get a shot.
If you have ever had an immediate allergic reaction to another vaccine or injectable therapy, you should consult with your doctor to see if it is safe to receive a COVID shot.
The agency said that people with a history of severe allergic reactions not related to vaccines or injectable medications—such as food or pet allergies—can still get the currently available COVID shots.
People with a history of severe allergic reactions or who have had any type of immediate allergic reaction to a vaccine or injectable therapy should be monitored for at least 30 minutes after receiving their shot, according to the CDC.
"Vaccination providers should have appropriate medications and equipment—such as epinephrine, antihistamines, stethoscopes, blood pressure cuffs, and timing devices to check your pulse—at all COVID-19 vaccination sites," the agency said.

Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Aristos is a Newsweek science reporter with the London, U.K., bureau. He reports on science and health topics, including; animal, ... Read more