Schizophrenia could be treated with cheap, accessible anti-inflammatory drugs like ibuprofen, according to new research.
The study, published on Friday in the American Journal of Psychiatry, concluded that patients suffering from schizophrenia showed high levels of inflammation in their brains They also discovered that people with other markers for a heightened risk of schizophrenia were likely to have higher-than-normal inflammation levels.
The findings suggest that, if detected early enough through brain scans, schizophrenia could potentially be prevented or at least mitigated in at-risk patients using simple anti-inflammatory drugs.
Peter Bloomfield, a doctoral student at the Medical Research Council's (MRC) Clinical Sciences Centre and the paper's lead author, says that the findings could change the way schizophrenia is diagnosed and treated. "There's potential for us to treat very early," says Bloomfield. "Also, this is a completely new type of theory of schizophrenia, so a whole new range of medication could be produced based on this research,"
He adds that over-the-counter medication —"something like ibuprofen or just any anti-inflammatory"—could be used to treat the mental disorder in the future, subject to clinical trials.
Schizophrenia affects more than 21 million people worldwide, according to the World Health Organization (WHO). Despite the fact that it is treatable with anti-psychotic medication and psychological therapy, the WHO said that one in two sufferers do not receive treatment for the condition.
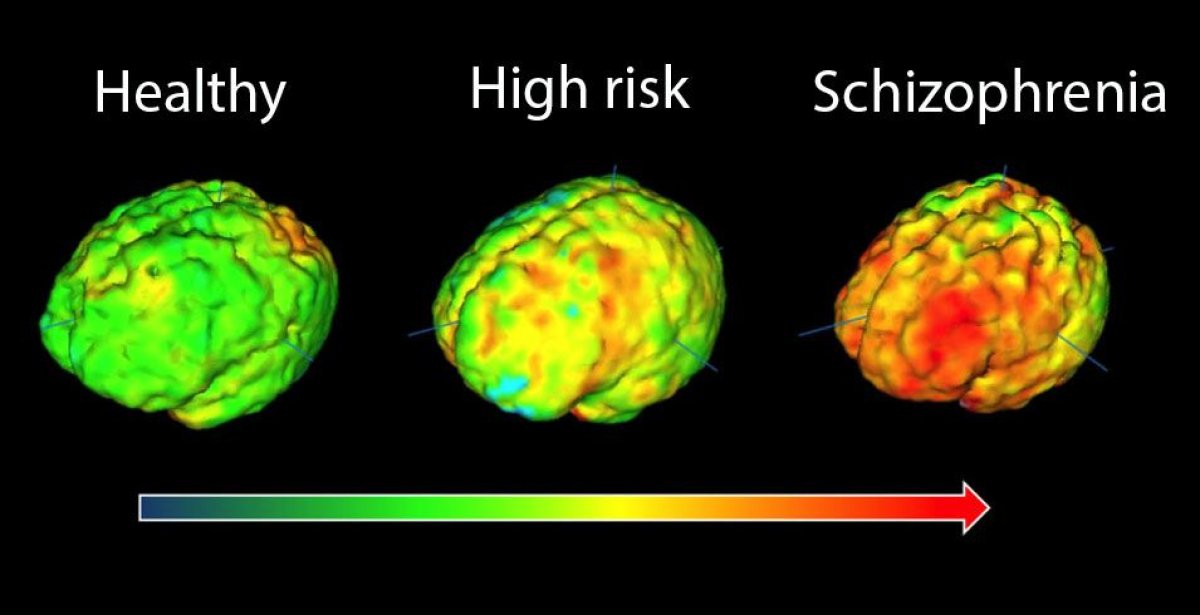
The recent study assessed the levels of activity of a type immune cells in the brain known as microglia of 56 patients in total, including current sufferers of schizophrenia as well as those at risk of the disease. Researchers injected the subjects with a chemical dye that sticks to microglia, which they then used to record the activity levels of the cells.
Microglial cells are the primary immune cells of the brain and spinal cord (or the central nervous system), where their function is to destroy pathogens and clean up debris. The cells also prune connections between brain cells, known as synapses.
Bloomfield explains that abnormal activity levels in microglia can lead to patients developing symptoms of schizophrenia—including hallucinations and delusional thoughts—by changing the way the brain is hard-wired. "If they're over- or under-active or active in an inappropriate way, then you would end up with the wrong number of synapses or inappropriate connections between different parts of the brain, which would fit very well with our hypothesis of how schizophrenia is actually manifesting," says Bloomfield.
Oliver Howes, head of the MRC Clinical Sciences Centre's psychiatric imaging group and the paper's senior author, told Sky News that the advance was the most significant in schizophrenia research for decades. "We're still using treatments that were essentially first developed in the 1950s and we desperately need new avenues and new approaches," said Howes.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
Conor is a staff writer for Newsweek covering Africa, with a focus on Nigeria, security and conflict.
To read how Newsweek uses AI as a newsroom tool, Click here.








