At 73, Kanta Patel is contending with a host of chronic health conditions. In 2004, she went for a physical and learned she had elevated cholesterol. Then, two years later, Patel's doctor diagnosed her with hypertension. She's also a borderline Type 2 diabetic.
One would never think Patel, who emigrated from India 50 years ago, had such serious illnesses. She appears fit: 5 feet tall, 102 pounds, with a body mass index of only 19. She has always been physically active, and she eats a vegetarian diet. But looks (and a great BMI number) can be deceiving.
An increasing amount of research shows that BMI and weight are not necessarily the main indicators of a person's health. Additionally, what's considered an unhealthy BMI—a number that may predict the onset of chronic diseases—is not the same across all races and ethnicities. Many who question the use of BMI in clinical settings point out that it's a health metric that's resulted from decades of research mostly conducted on white people.
However, regardless of family ancestry, BMI and weight are often the first numbers doctors consider, and they may not screen for heart disease and Type 2 diabetes if they are within normal range. A large study based on more than 40,000 people published in the International Journal of Obesity suggests that nearly half of the people categorized as overweight were cardiometabolically healthy, while 30 percent of people within the normal BMI range were not in great shape.
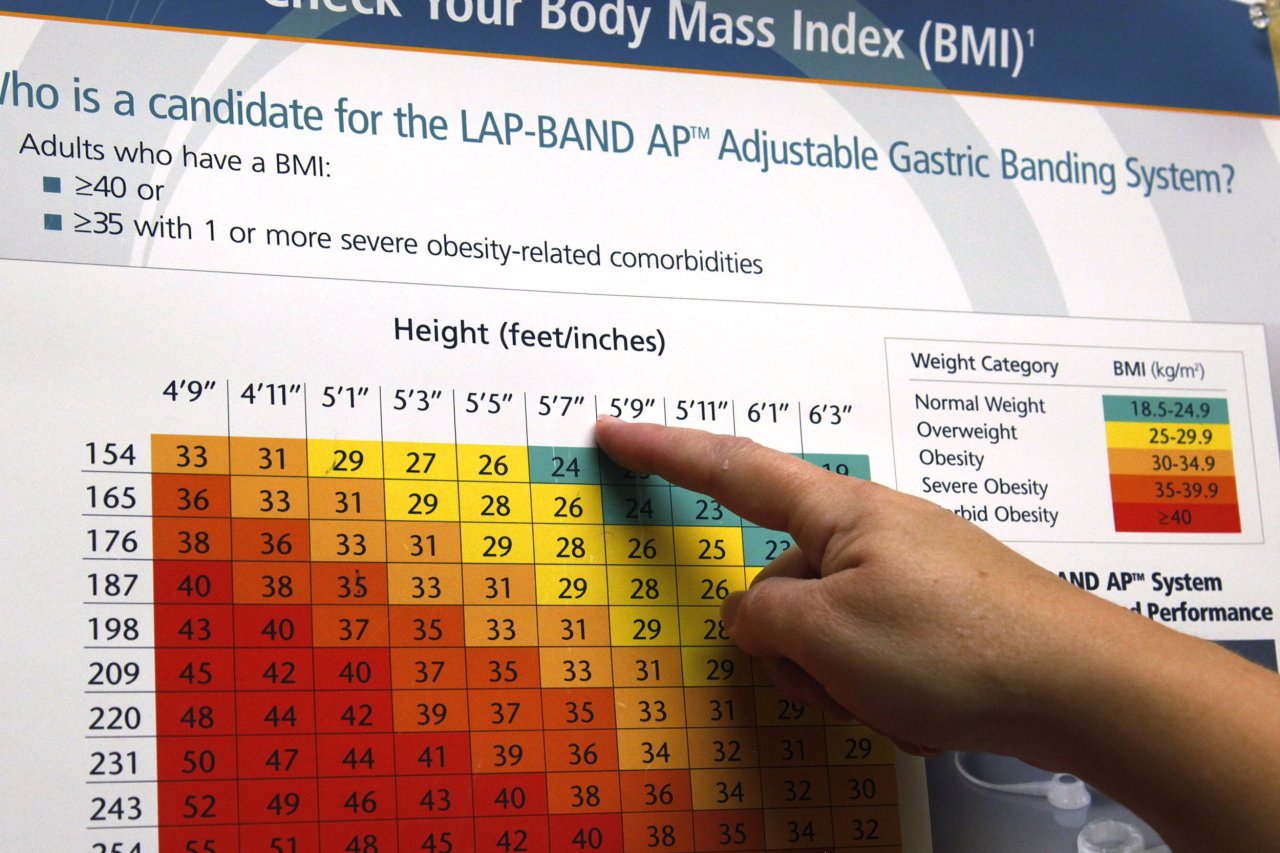
The U.S. Centers for Disease Control and Prevention and other public health authorities say a healthy BMI for adults is between 18.5 and 24.9. (An adult with a BMI between 25 and 29.9 is considered overweight, while someone with a BMI of 30 or above is classified as obese.)
Dr. Alka Kanaya, a professor of medicine, epidemiology and biostatistics in the division of internal medicine at the University of California, San Francisco, is among the many experts who say glucose and cholesterol screening should start sooner for patients within standard healthy BMI ranges to improve early detection. "You might not miss many whites if you wait until their BMI is 25, but you will miss other race and ethnic groups if you wait that long," says Kanaya.
A recent study co-authored by Kanaya suggests Americans of South Asian descent who have BMIs within the healthy range are two times more likely than whites with similar BMIs to have an increased risk for heart disease, stroke and Type 2 diabetes. In 2014, the American Diabetes Association revised its screening guidelines for Asian-Americans. The organization now recommends doctors begin screening patients in this group with BMIs of 23 or higher for diabetes, rather than the standard clinical practice to start testing at 25 or above.
This is the first study of its kind based on patients from five racial and ethnic groups. Published in Annals of Internal Medicine, it involved 803 South Asians in the San Francisco Bay Area and Chicago whose family ancestries could be traced to India, Pakistan, Bangladesh or Sri Lanka. In addition, the researchers examined data from a study of some 6,000 participants from New York, Baltimore, Chicago, Los Angeles, Minneapolis-St. Paul and Winston-Salem, North Carolina; the diverse pool included Chinese, Hispanic, African-American and white people.
The researchers discovered that the cardiometabolic risk factors for a white person with a BMI of 25 appeared at much lower BMIs in patients from other groups: 22.9 for African-Americans, 21.5 for Hispanics, 20.9 for Chinese and 19.6 for South Asians. After controlling for lifestyle factors such as smoking, alcohol intake, exercise and diet, they found that only 21 percent of whites had cardiometabolic risk factors but normal BMIs, whereas 39 percent of Hispanic-Americans and 44 percent of South Asians had a normal weight but a higher risk for chronic diseases that are usually associated with being overweight.
Early diagnosis of Type 2 diabetes and cardiovascular disease is critical to saving a patient's life. However, health experts disagree on when screening should start. The U.S. Preventive Services Task Force, for example, strongly recommends screening adults for Type 2 diabetes aged 40 to 70 years old who are overweight or obese. The American Diabetes Association recommends that all adults—regardless of weight—have blood sugar measured every three years starting at 45. Both expert panels acknowledge that certain racial and ethnic populations are at higher risk for the disease, so they advise doctors to consider this when determining when to start screening patients who are not overweight.
The other problem, Kanaya says, is that BMI doesn't consider where fat is distributed in the body. Her study found that "fat in the wrong places"—the middle and around the visceral organs, in the liver and around the heart—were a leading indicator of metabolic syndrome that vastly increased risk for Type 2 diabetes and heart disease.
It's well established that obesity is a leading cause of cardiovascular disease and Type 2 diabetes. But the problem is far more complicated than that, and in ways scientists are only just beginning to understand. Certain genetic variants put skinny people at higher risk for developing obesity-related diseases, and these mutations often cluster within certain racial and ethnic populations. But there's also something even more complex at play—epigenetics, or the external modification of genes.
Studies find that when genes become altered by outside influence, the mutations can be passed on from parents to offspring. This may be one reason why some diseases become endemic to certain racial or ethnic groups. A study on mice published in Nature Genetics in 2016 suggests that the diet a parent eats—especially one that is high in fat—can actually influence the glucose tolerance and obesity risk of offspring. In the study, the researchers carried out in vitro fertilization with sperm and egg cells from adult mice in three diet groups: high-fat, low-fat and normal (control). Fertilized eggs were placed in healthy surrogate female mice. They found that the mice conceived from parents in the high-fat diet group had higher glucose intolerance than mice from the other groups. They also tended to be more overweight.
Kanaya suspects that factors such as high levels of stress and exposure to pollution and toxins are also prompting some modification of genes. In her study, for example, 98 percent of the South Asians and 96 percent of Chinese people had immigrated to the U.S., an experience that often brings trauma and significant changes to living conditions. "It's both a combination of environmental factors, whether it be lifestyle factors or possibly other factors that people have been exposed to through their life course," says Kanaya. "That can then lead to more aggressive or earlier diseases at lower body weights."
The BMI equation has its origins in the mid-19th century, when it was first conceived by Adolphe Quetelet, a Belgian mathematician, astronomer and statistician. Quetelet did the simple math—ratio of kilograms over height squared—to define the characteristics of a "normal man" and eventually as a way to spot epidemiological trends. The eponymous mathematical formula—the Quetelet index—wasn't named the body mass index until 1972, when American physiologist Ancel Keys wrote a paper on the subject.
Quetelet never intended that BMI be used to direct a patient's medical care. However, insurance companies have still put weight on the measurement, justifying higher premiums for people with higher BMI and less coverage (higher out-of-pocket expenses) for patients who have BMIs within the normal range.
Part of the problem is that BMI doesn't take into account factors such as the weight of bone and muscle mass as both compare to fat. People who are highly active are likely to have denser bones and heavier muscles, which can make it seem on paper that a gym rat is overweight or even obese.
In April, pop music icon Pink took to Instagram to poke the BMI paradox. It's indisputable that Pink, who is known for singing while performing circus-like acrobatics, is far from obese. For a selfie at the gym clad in spandex just after having her second baby, she wrote: "Would you believe I'm 160 pounds and 5'3"? By 'regular standards' that makes me obese."