More than a decade ago, Judy Van de Water, a neuroimmunologist, decided to follow her instincts and research a condition she knew nothing about. Van de Water, now a lead scientist at the University of California Davis MIND Institute—an international research center for neurodevelopmental disorders—had spent her career studying the immune system. In 2000, she stumbled upon a compelling area of research: the immunobiology of autism.
Through studies on mice, rats and rhesus macaques and, eventually, retrospective and prospective analyses of children diagnosed with autism and their mothers, Van de Water identified eight autoantibodies made by a mother's immune system that appeared to be linked with autism risk if they crossed the placenta. Van de Water, who is also a researcher in the department of internal medicine at UC Davis, refers to her discovery as maternal autoantibody-related autism, or MAR autism. The concept is controversial and became more so when Van de Water developed a test to measure those biomarkers in a woman hoping to conceive, thereby predicting her risk for having a child who develops autism.
After Van de Water published a paper in 2013 that identified those autoantibodies, a company expressed interest in licensing a patent from UC Davis for the test, and in marketing it. Van de Water says the test wasn't ready then but that the blood-based test is now 99 percent accurate at identifying a constellation of immune markers that contribute to autism risk. She hopes to make it available to families in a few years. "It's not just one autoantibody that gives you [the condition]. We're still figuring out which is pathologic and which one is just a biomarker," she explains. "You have to have a combination of them."
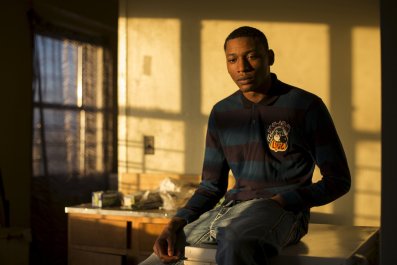
What she has observed in her research is that kids whose mothers have the main two biomarker patterns have the most severe form of autism. "They're usually not verbal. They have more stereotypic behavior." They also tend to score higher on the Autism Treatment Evaluation Checklist (ATEC), an assessment tool administered to parents, teachers and caretakers to evaluate a child and determine the severity of his or her condition.
Many experts caution that predicting autism risk is not as tidy an endeavor as research like Van de Water's might lead the public to believe. The concept of early diagnostic testing is appealing to some parents, but critics argue that such testing would be unethical, and that early diagnostic testing would only increase the fear and stigma already surrounding the condition.
Should Van de Water's test enter the market, women could opt to have it before deciding to conceive. Regardless of her test results, choosing to move forward with a pregnancy would be a personal decision. The same test could also be used postnatally to evaluate a child with developmental delays.
The current prototype of Van de Water's test has already guided some family-planning decisions. A few years ago, a couple that enrolled in one of her studies chose to have a child through a surrogate after the woman tested positive for that pattern of high-risk biomarkers. The couple already had one child with autism, and the risk of having an offspring with autism is roughly 18 to 20 percent higher for parents in those circumstances. Through the surrogate, the couple went on to have a child who has not developed autism. Van de Water says this particular case shows that her test would provide some level of assurance when making difficult and life-changing decisions about starting a family.
Rates of autism continue to rise. The U.S. Centers for Disease Control and Prevention estimates that currently 1 in 68 children in the U.S. is diagnosed with autism. In 2008, approximately 1 in 88 received an autism diagnosis. That trend leaves many people wishing for a more exact way to assess a child's risk for autism, or at least provide early preparation for services a child with neurodevelopmental problems will need.
However, autism spectrum disorder is a complex condition influenced by factors related to biology, genetics and environmental exposure. Genetic research alone has pinpointed some 50 genes that appear to be linked to autism risk, and there are likely many others. But mutations don't guarantee that a child will develop the condition, and many experts agree that it would be dangerous to rely on the results of any test—regardless of which biomarkers it is able to measure—in order to make difficult decisions about a pregnancy or to determine a child's level of care.
"I think the first question you have to ask is why are you doing this, what benefit are you offering to the family and that child," says Stephan Sanders, an assistant professor of psychiatry at University of California San Francisco. "If the answer is you have a treatment and it's going to make a difference, even in a tiny percentage, then I think such things are a welcome and useful idea. If the answer is you're just giving bad news, then it's hard to see who you're benefiting by doing that."
Children with autism usually receive a diagnosis between ages 3 and 4, at which point they begin receiving care. In many cases, a child won't exhibit symptoms (or they'll go unnoticed) until the first few years of life. But some experts assert that diagnosing and treating a child even earlier can mitigate many of the common symptoms. For some, that's reason enough to develop a precise way to evaluate autism risk. Tests like Van de Water's could be used to assess children in the first year or two of life who are not reaching developmental milestones, especially as a growing body of research continues to show that early intervention makes all the difference.
One study, published in 2014 in the Journal of Autism and Developmental Disorders, found that children who received interventions through a 12-week treatment program in the first year of life had fewer language delays and developmental problems associated with autism. Earlier intervention was highly effective: Six out of seven kids caught up with non-autistic peers on developmental milestones by age 3 or 4.
Other researchers have attempted to create tests that can aid in diagnosing children earlier. Between 2010 and 2015, Theresa Tribble worked as a head of commercial strategy for SynapDx, a now defunct laboratory services company that attempted to create diagnostic tests for the early detection of autism spectrum disorder. With $9 million in venture capital, the company set about developing a blood-based test that could identify a certain set of biomarkers linked to autism. SynapDx hoped the test could be used as an assessment tool for infants and toddlers showing signs of developmental delays, so they'd get earlier intervention and treatment.
SynapDx set up a large-scale study that involved 800 autistic children at 19 sites across U.S. and Canada. The company experimented with tests that analyzed DNA, RNA, metabolites and other biomarkers to determine which ones correlated with autism. But Tribble says the study failed to prove its potential to be both reliable and accurate, and the company shut down.
Lauren Flicker, assistant director at the Montefiore Einstein Center for Bioethics and assistant professor in the department of epidemiology and population health at Albert Einstein College of Medicine, says any diagnostic test wouldn't provide the whole picture. "In some ways, it seems like parents should get all the information they can, or at least they have the right to get all the information they can," she says. "The child may or may not develop autism, and the child might lie anywhere on the spectrum."
While most children and adults with autism exhibit at least a few of the classic signs—repetitive behavior, difficulty with communication and social interaction, obsessive interests—plenty of people with autism are high-functioning adults. "We don't want to be doing eugenics," says Sanders. "We don't want to be removing a group of diverse people who we want to embrace in society."
Flicker says a reliable diagnostic test could theoretically be utilized for in vitro fertilization. In IVF, fertility clinics already run a number of test on embryos to identify the healthiest ones, ruling out rare genetic diseases such Tay-Sachs, cystic fibrosis, blood disorders such as sickle cell anemia, spinal muscular atrophy and Fragile X Syndrome, a condition that causes intellectual disability (that frequently goes hand in hand with autism spectrum disorder). A test that predicts autism risk would simply be a way to rule out severe abnormalities.
"It's great to have information," says Flicker. "We make choices based on thoughtful consideration of information, but this isn't hard data. It isn't telling us any information about what children will be like."