Updated | Early on a recent morning, woodsmoke wafted above the murmur of village life in Gorama, Sierra Leone, as Rupert Allan sat sweating in the shade of a concrete veranda. A member of Missing Maps—a humanitarian project that maps parts of the world vulnerable to natural disasters, conflicts and disease—Allan tapped away on a small laptop next to a black goat and a small, tame monkey. Connected by a smartphone hotspot, Allan was in charge of mapping the nearby area.
This summer, the Missing Maps team spent months traveling to remote parts of Sierra Leone by motorcycle to chart them for the first time. Despite the ubiquity of Google Maps, there are many places on Earth where people and the terrain they live on haven't been mapped. Globally, over a billion people are unaccounted for—literally not attached to a physical address in cartography or databases, which means they often don't receive basic services. That number is growing; by 2020, there will be 1.5 billion people living in slums, the majority of whom are unmapped. Accounting for these people is important not just to better understand our world but also because there's a direct link between people being not accounted for on maps and the risk of catastrophe for them—and, as the Ebola outbreak demonstrated, for the rest of us.
Ivan Gayton, the founder of Missing Maps, says his crew ventured so far into the bush in Sierra Leone this summer that even local team members were sometimes astonished when they came across villages where their maps had showed blank spaces. "You're watching light dawn in their eyes, as they see no one has ever been here—no one has ever cared enough to come here," he says. "There's just people living in the forest hacking their own roads with machetes, essentially unknown to anyone."

Gayton first became interested in cartography in 2010 when he was battling one of the worst cholera epidemics in history in post-earthquake Port-au-Prince, Haiti. Then a field logistician for Doctors Without Borders, Gayton and the other medics in Port-au-Prince asked all the patients who walked in where they lived. But because the team didn't have accurate maps of the city, they couldn't send help—to trace contacts or find other sick people—to the right places.
Knowing where patients are coming from, and therefore being able to track the progress of a disease spatially, may seem like common sense now, but modern epidemiology itself is comparatively new. It wasn't founded until 1854, when Dr. John Snow mapped an outbreak of cholera in London. The developed world has since taken spatial epidemiology—the study of the distribution of health outcomes—to an extreme. By comparing geographic data to medical records in Europe and the United States today, health workers can now predict life expectancy by mailing address. But in vast swaths of the world, it's still impossible to trace disease outbreaks even the way Snow did more than 150 years ago, because there are no accurate maps.

Back in Haiti, feeling desperate about the fast-moving epidemic, Gayton asked Google to help chart which slums had cholera patients—"like calling the Bat Cave," he jokes. Luckily, Google was already working with earthquake disaster relief, like the Humanitarian OpenStreetMap Team that had been mapping destroyed areas of Port-au-Prince. With the use of these new maps, Gayton was able to pin where groups of patients were coming from and identify potential contamination sources, such as infected wells. The effect was like magic, he says. "The conversion rate instantly turned around."
This success spurred Gayton to help organize a map-making collaboration between tech-industry volunteers like Google and OpenStreetMap and nongovernmental organizations like Doctors Without Borders and the Red Cross. Missing Maps now regularly holds "mapathons," in which volunteers look at satellite photos to find towns and villages in regions at risk of disease or conflict. That data are then sent to locals in those areas, who often go out with printed copies of the satellite images and label street names and neighborhoods in their own language. (To be useful, the maps have to be locally relevant. Imagine a doctor trying to locate a patient in a slum without knowing how to spell or even pronounce the street names.)
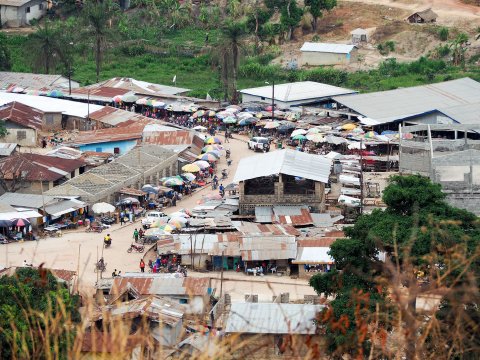
Over the past few years, Missing Maps has made much progress, but in many places satellite photos are either obscured or inaccurate. That's why Gayton decided to privately fund an expedition to Sierra Leone this summer, collecting donations but mostly paying out of his own pocket. For weeks, a small team on motorcycles mapped remote parts of the country and trained locals to use their smartphones and bikes to record geographic information about their environs. All that spatial data will be connected to local place names and then shared online. Since Sierra Leone was part of the Ebola outbreak in 2014, says Gayton, "ultimately our proof of concept is that we make a map that will [be able to] stop Ebola. I like maps, but what I care about is access to health care. The outcome I'm looking for is tangible evidence that it helps saves lives."
A review recently published in the International Journal of Epidemiology found that the lack of spatial data was, in fact, a key factor in West Africa's Ebola outbreak. "Infectious diseases have a spatial structure," the author, Tom Koch, writes, so mapping these areas has become a low-tech race against time—and the next epidemic.
Gayton's already putting his initial data to use in collaboration with Dr. Ed Monk, a visiting resident at a small hospital in Segbwema, a town in eastern Sierra Leone that serves 30,000 people. "As soon as you walk on the wards, you can tell there's been a better time for the hospital," Monk says. When Segbwema had a bustling diamond mine, it was the home of a renowned Lassa fever virus center, but during the civil war on and off from 1991 through 2002, the railroad was gutted and the hospital where Monk now works was temporarily closed. Today, the old water tower outside the hospital has a shrapnel hole through it, and the wards are sprawling rows of cots with improvised mosquito netting. But what the hospital does have is surprisingly good patient records, thanks in part to Gayton's efforts.

This summer, Gayton mapped all the dwellings in the catchment area, finding 3,000 hamlets by going door to door and "asking them, 'What do you call this village?'" He produced a gazetteer, a map with both statistical and geographical information, for the hospital registrar. Now, when patients come in, their homes can be identified on a map.
Ka-Ping Yee, a former Google software engineer who visited Port-au-Prince in 2010, came to the hospital to help train the staff on how to use the gazetteer. Ping also built a program to collect medical data, making it possible to track where patients are coming from. "Let's say one village has so many malaria cases," says Solomon Musa Vandi, the principal of the nursing school. "We go there, we find out why. That's what we lacked in the time of Ebola in this country. If people had this sort of facility, that disease would not have spread."

Gayton's team in Sierra Leone has, of course, run into challenges, large and small. In June, a team on motorcycles was very deep in the diamond hills, after hand-poling a ferry across a river and navigating flooded roads where the bikes were up to their gas tanks in water. A team member came down with a fever. "In the back of my mind, I was thinking, If he gets worse, what do I do? There's no one to call," says Allan. They mapped the village, and the stricken man, shaking with malaria, had to be held upright on the back of a motorcycle for the return trip.
The team also had to struggle with the enormous physical challenges of a technologically sophisticated project in a country where neither electricity nor network signals are reliable. "We're building a playbook so anyone else in the world who wants to can replicate it," says Gayton, who's kept careful logs of the process. "This is how much it costs, this is how much we pay mappers, this the technology, the training manuals—you can just adapt it to the local context. I have one goal from this, and it's to get the rest of Africa mapped."
The communities Missing Maps are working in are often isolated and undereducated, far from government oversight or opportunities for education—places where, when something goes wrong, people have small chance to recover. "Local names are important," Allan says. "Geotags are critical. Terror spreads as fast as the epidemic itself in these communities."
He pauses. "The enemy is the unknown."
Corrections: A previous version of this story misspelled Rupert Allan's name.
A previous version of this story referred to Solomon Musa Vandi as a community health nurse at the hospital. The story has been corrected to state that Vandi is the principal of the nursing school.