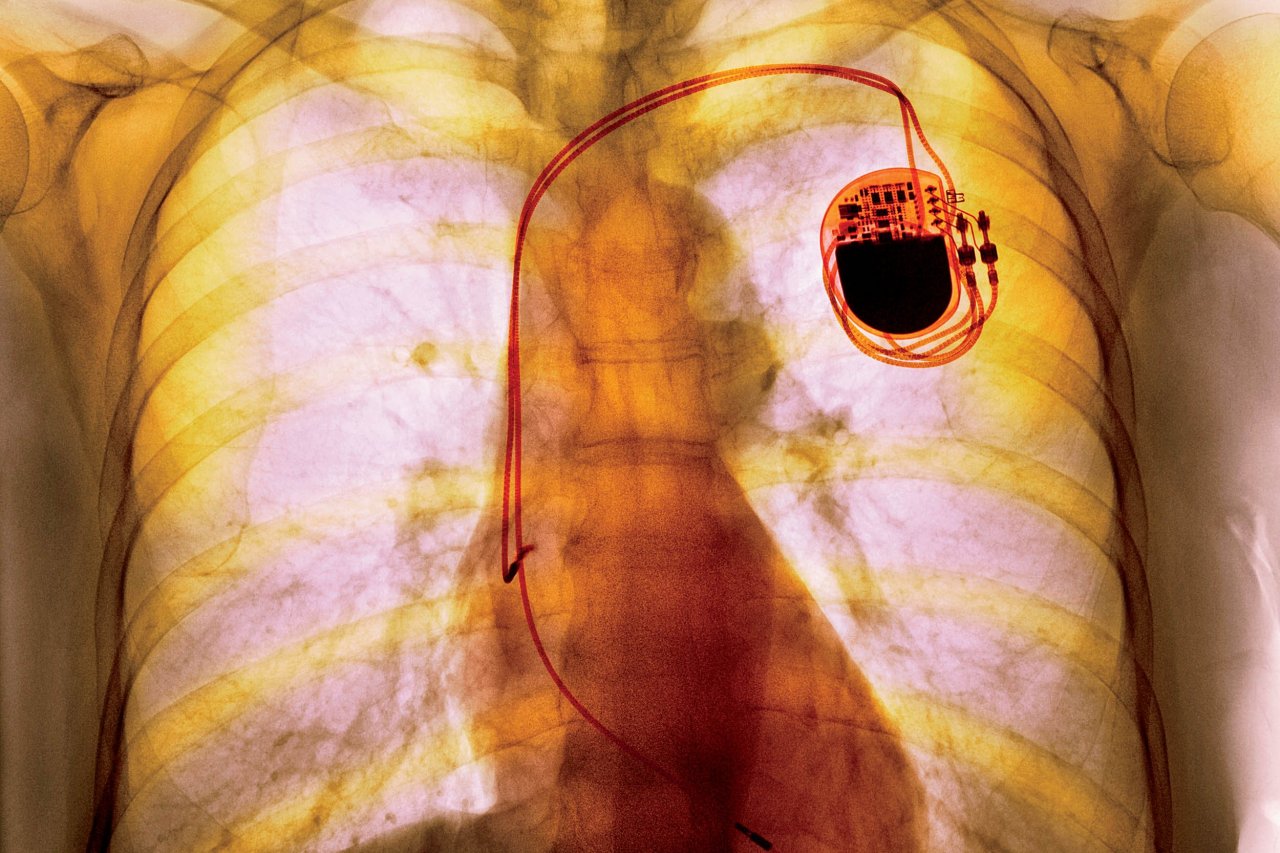
Pacemakers are big: They're about the length of your pinky finger and weigh an ounce, with batteries taking up most of that real estate. And size matters: Large cardiac implants can lead to infections, muscle tears and lead fractures or perforations.
These bulky devices may soon be a thing of the past, as researchers at Stanford have developed a new form of wireless power transfer that will make it possible for implants to have much smaller batteries. Ada Poon led the team that recently announced it had built a pacemaker smaller than a grain of rice using this technology and had implanted it in a lab rabbit.
To power the tiny pacemaker wirelessly, researchers needed two types of electromagnetic waves—far-field and near-field—to penetrate deep into the body. Radio towers emit far-field waves, which can travel over long distances, while near-field waves travel over shorter distances and are used in hearing aids. But neither one is completely safe or effective in biological tissue: Far-field waves are reflected off or absorbed by skin, while near-field waves can't travel very far inside the body. Poon's team found a "sweet spot" by combining the two wave types to produce "mid-field" waves. The technique uses just about the same power as a cellphone but at levels well below the dangerous exposure minimum for humans.
"We're not the first to do wireless power transfer," John Ho, a Ph.D. candidate in electrical engineering at Stanford who assisted in Poon's research, tells Newsweek. "It's been around since the early 20th century. So what we've done is look into different ways to set up ways to permeate biological tissues."
The researchers believe their technique could power tiny devices placed nearly anywhere in the body, with almost limitless potential—they could stimulate nerves and implant sensors that monitor a person's vital functions. The method allows the researchers to get to places in the body "not previously reached," Poon says. "One of the most promising things is the idea that certain diseases would be better treated by changing neural activity and pathways rather than using drugs," she tells Newsweek. Electroceutical treatment would directly modify brain circuits and target specific parts of the body, rather than "change the global body on a chemical level" the way drug therapy does. The technique could help treat disorders like Parkinson's, Alzheimer's, urinary incontinence, chronic pain and arthritis.
The researchers are hoping to test the method in humans in the next year, but it could take another five to 10 years to be deployed clinically.