Evan Rose's cancer should have killed him.
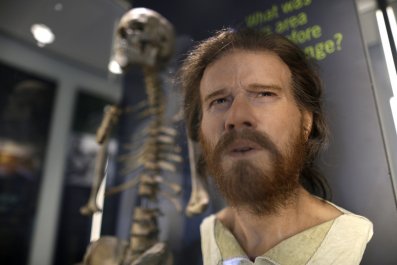
The surgeries to remove tumors that grew in his throat because of his sarcoma left him without a larynx. He now breathes through a hole in his neck, a stoma, and when he speaks he sounds as if he has a nasty case of laryngitis. In a raspy whisper, while pressing a button in his throat to close the stoma so he can create sound, Rose describes the doctor's initial response to the outlook for his cancer—a type so rare that there are only 200 known cases worldwide—as grim. "They didn't want to do anything dramatic if I wasn't going to live that long," he recalls.
It has been seven years since that initial diagnosis. The slow and steady march of innovation in our understanding of cancer and the emergence of companies providing personalized treatments have not only saved Rose's life but allowed him to turn his cancer from a death sentence into a chronic illness that simply needs regular managing. A mere annoyance. "Yes, there's all this cancer stuff that I deal with," he says. "But for the most part I live a pretty normal life."
Rose is alive today thanks to personalized medicine. But not the kind that typically comes to mind. That term has become so generalized that many in the medical industry have started replacing it with "precision medicine" to avoid confusing it with the notion of doctors spending an extra 30 minutes with their patients and calling their care "personalized."
No, this precision treatment comes thanks to advances in genetic screening and the ability to run a genome sequencing on patients—allowing doctors to see inside one person's disease and determine how he or she fits into a set of patients with illnesses that match the person's disease on a molecular level. In other words, no one just has "lung cancer" anymore. Patients are now diagnosed with a certain type of lung cancer defined by the genetic makeup of their tumor.
It's important because doctors are finding that diagnosing someone with a disease often isn't enough to find the right treatment. Everyone's body is different, and not all methods for healing are going to work. Think of it like this: Every disease is a bag of Skittles. Inside the bag are lots of different flavors. They're all still Skittles, but they're not quite the same—you can separate them out into groups of flavors, or subsets, if you will.
Treating diseases this way isn't easy, and not all illnesses have the molecular differences that allow them to be eliminated so specifically. But researchers are working hard to find ways to develop new methods for the ones that can.
Diabetes is one common disease that could respond to precision medicine. It's characterized by high glucose levels in the blood that aren't naturally eliminated by the body (either because there is a lack of insulin or because the body's organs can't use insulin to remove excess sugars). This is easily treated for some people, but others develop serious symptoms—and may even lose their vision or need to have limbs amputated. If doctors were able to use genetics to identify who might develop higher-than-normal glucose levels and respond negatively, they could target and treat vulnerable patients sooner. Researchers are also looking into rheumatoid arthritis and multiple sclerosis, attempting to find biomarkers and proteins that can set different patients apart.
But studies on these diseases aren't very far along. That's because they're so complicated—in cases like diabetes, scientists will need to look at all the possible genetic and nongenetic factors that can affect the disease (age, body-mass index, how long patients have had the disease and their genetic tendency to respond to treatment). Cancer is where precision medicine really shines, because of the nature of tumors. As a cancer cell replicates, it generates mutations in its DNA. Those mutations are what causes the tumor to grow out of control. And all cancer mutations are not created equal. For every type of cancer there is a subset of mutations. If doctors can run a genetic test on a person's tumor and understand the specifics of that growth, they can pick the right kind of drug to fight it.
It sounds simple, and maybe even a little bit obvious, but it's a revelation. According to Chuck Baum, the former head of oncology for Pfizer, treating cancer used to be completely generalized. For example, in 1999 he developed a drug for combating brain cancer. "It was for the minority of patients that would benefit. But we never knew who they would be. So we'd treat everybody [with it]," he says.
That's an awful way to treat patients—it's almost like running an experiment on humans. Cancer drugs are extremely toxic; even when they work, they can ravage the body. And more often than not, there is little to no effect on the cancer. People get sicker from the attempts to make them healthier. "We just didn't understand the disease well enough," says Baum. "There wasn't enough information."
There was no protocol to fight Evan Rose's cancer when he was diagnosed in 2007, which meant his doctors had to invent one. That's another common problem with the old "one drug to treat them all" method. A doctor diagnoses a patient with, say, lung cancer, then looks into the options. Maybe there are studies that show a given drug will benefit lung cancer patients and other studies that show it won't. There might be professional hypotheses that the drug will have an effect in cutting off blood supply to a tumor, but it's likely that it'll be a controversial idea.
"Cancer is largely based on empiricism," says Dr. Robert Maki, Rose's oncologist at New York's Mount Sinai Hospital. "You can catalog these experiences, and that's what we use as a playbook to decide what to use to fight cancer."
But Rose's cancer was so rare, there was no literature to look at; Rose and Maki had no choice but to turn to precision medicine to help them identify the right treatment. So they went to Champions Oncology, a company leading the field of personalized cancer medicine.

Of Mice and Sick Men
The goal at Champions is to find the right drug for patients based on a tumor's unique reaction to different chemotherapies. It does this by taking a section of the patient's tumor and implanting it into mice bred without an immune system (which allows scientists to see exactly how the drugs will fight the tumors without having to determine if the drug is making the difference or the mouse's immune system is). Then they test a slew of drugs and drug combinations on each mouse to see which best fights the patient's tumor.
The company began as an outgrowth of research undertaken by physicians at Johns Hopkins University. They were frustrated by how rarely cancer drugs seemed to be effective in treating the disease. "One of the major problems with pre-clinical models for cancer drugs is that 85 to 90 percent of them that show benefits in animal models weren't translating to humans," says Dr. Ronnie Morris, president and director of the company. "How was it possible all these tens of millions of dollars in cancer drugs didn't work in the clinic?"
Morris says that the testing models that scientists had been using for the past 20 years or so were all based on clones of the most aggressive tumors—and didn't take into account the complexity found in the cancers of actual patients. "They would find a drug to kill it and say they have the best drug," he says. "Then they would go into the clinic and it wouldn't work."
Champions's model is entirely different: Instead of testing a 20-year-old cell line, it tests the cells of the patient herself. "What we do is we simply take the tumor out of the patient. It grows as a human tumor in a host environment. Then we can do experimentation and test different therapies to see which is the most effective," he says. Instead of subjecting a patient to toxic chemotherapies, the testing happens outside the body.
Once a large enough piece of the tumor is removed, it's shipped to the nearest Champions lab within 24 hours. The tumor is then dissected into several small pieces and implanted into the flanks and renal capsules of mice. (The number depends on how many cancer treatments the patient's oncologist chooses to test.) Then the tumors are allowed to grow until they can be biopsied again and reimplanted in a much larger group of mice—usually between 20 and 30—which will be separated out into a control group and a group for each of the different drugs and drug combinations. Then the testing—tailored to the specific needs of the patient—can begin.
In June 2012, Rose and his wife, Josslyn Shapiro, along with Maki, decided to work with Champions. After years of surgeries to remove his various tumors, Rose's cancer "was back with a vengeance," he recalls. Doctors had already done genetic sequencing on growths in his neck, and although they found a specific mutation and tried two different drugs to target it, neither had worked. In the meantime, the chemotherapy had been toxic enough that he had temporarily lost his vision, his hair and his ability to walk. "I even lost my eyebrows once," he says.
They had sent a small piece of the tumor to Champions previously with the hope that it could be propagated, but there wasn't enough. "The day before Evan was going to have the entire tumor removed from his neck I called them as asked if they wanted it. They said: "Yes, yes, yes!"' says Shapiro. So, working with Maki and three other oncologists, Rose came up with a list of eight different drugs he wanted Champions to test on his tumor.
While they waited for the results—it can take four to six months—Rose got worse. "I got really sick. My lungs were filling with fluid. A tumor had grown out of my lung," he says. "One of my doctors said, 'If we can't find a chemo that works, you probably won't make it through the year." The mouse avatars growing in the lab at Champions were his last hope.
Then there was the good news: One of the drug combinations Champions had been testing was having a dramatic effect on the mice. Rose's cancer was sarcoma—one of the rarer types that typically grow in soft tissues like muscles and blood. The combination of drugs that seemed to work best was commonly used to treat sarcoma in children. And that meant Rose's anatomy was different from the bodies the drugs were designed to work in. They made him extremely sick, and his doctors had to draw out the treatment—15 minutes of IV therapy every morning and "two really big pills" at night, every day for five days. Then a week of being very sick. Rose did this every three weeks for a year. The tumors began to shrink. "All of my doctors were jumping up and down. They were excited and said, 'We've never seen this in sarcoma,'" he says.
Rose was alive, and the team had a new plan to fight the tumors. Because they eventually would mutate and the drugs would stop working, Champions would now be integrated into the routine: Cutting out the big tumors that were surgically accessible and using Champions to find the right drug to treat the mutated tumors that remained. "My cancer, because it's so rare, it's the perfect thing for Champions. If you have a common cancer, there have been a million clinical trials. There's a lot of protocols to treat it, and they generally have some ideas what to do. For the past seven years, I've been a guinea pig. Seven. And it's kind of crass, but I'd rather have the mice be the guinea pig than me," Rose says.
Stay of Execution
One of the major drawbacks of this type of treatment is that it's extremely expensive. Insurance doesn't pay for off-label use of cancer drugs—even if Champions's scientists are able to prove they will work. Rose and Shapiro wouldn't say how much they paid Champions to find the perfect drug. "Let's just say it was a lot of money and I felt lucky that I have the resources to be able to do it," says Rose. "There's no doubt that part of me feels a little guilty that others don't have the ability to do it."
His oncologist, Maki, says he hasn't been able to treat many patients with this method because of the cost. "It's an expensive technique right now, and the people with cancer have been footing the bill. I haven't been able to find that many people for it. You could easily run up a tab of $50,000 to $100,000."
Even simple genetic testing on a tumor to determine the type of mutation can cost $500 to $10,000, he says. But these prices are going to start coming down as more companies get into the business. Baum, who left Pfizer to start his own company developing cancer drugs targeting specific tumor mutations, says it's very possible that in five to 10 years, precision medicine will be the only way cancer is treated.
Genetic testing on tumors is already starting to become the norm. In the big cancer hospitals like Sloan-Kettering, Dana-Farber and MD Anderson, all incoming patients automatically have their tumors sequenced. And in some cases insurance is beginning to cover the costs.
Meanwhile, precision cancer diagnosis and treatment is growing into an industry. Companies like Foundation Medicine are beginning to do genetic analysis on tumors. Edico Genome has created a small chip that helps testing companies manage the huge amounts of data that come from creating tumor genomes. Clovis Oncology, like Baum, is getting into the game of targeted drugs. And a nonprofit called the Clearity Foundation, created by a scientist who was diagnosed with ovarian cancer and was shocked that no laboratories at the time were profiling her type of disease, has emerged to help newly diagnosed ovarian cancer patients understand what types of molecular methods are available to them.
It has been said that the best way to survive cancer is to hold off dying long enough that a new treatment can be invented to save your life. That seems to be true now more than ever. Of course, for many cancer is still a death sentence. But Rose is a clear example that it doesn't have to be. Through seven years of toxic chemotherapies and countless surgeries, he has never left his job (in fact, today he has three jobs—he's the founder of San Francisco design firm SITELAB urbanstudio, a professor of practice in the Department of City and Regional Planning at the University of Pennsylvania and is running Urban Design+, another design firm, based in New York City). During his treatment, he and Josslyn even had a son, Ryder, now three and a half years old.
In many ways, Rose is living with cancer the way someone with HIV/AIDs would have shocked the world by doing so 10 years ago. The disease, once thought to be a debilitating death sentence, has become something that just needs regular care. According to Shapiro, "Before, when we were told there was only palliative care and they told us the best they could do was manage his disease, I thought that was a failure. But actually, it's not a failure. You can live with disease in your body."
When Newsweek talked with him, Rose was getting ready to head back into the hospital for surgery to remove yet another tumor or, as he says, "do some debulking." Asked if he ever thinks about giving up, he answers, "Why would I do that? We have an amazing son. I have a great life. It's full. For me, this cancer is an annoyance. It's a pain in the butt. It's inconvenient. I look at it as a chronic disease that I have to manage.… Every year they're coming up with new things. Every year that I'm alive there's more opportunity. I fully anticipate being here to see my son get married. I have no doubt about it."