In 2004, Danielle Decrette went in for in vitro fertilization. It wasn't her first time—she and her husband had a 3-year-old daughter conceived through IVF—and she knew what she was getting into. Just as he had four years before, Decrette's doctor stimulated her with hormones, extracted her eggs from her ovaries, fertilized them with sperm in the lab and placed the resulting embryo in her uterus. But this time the process failed. So the doctor decided to transfer two embryos in the next round to increase her odds of getting pregnant.
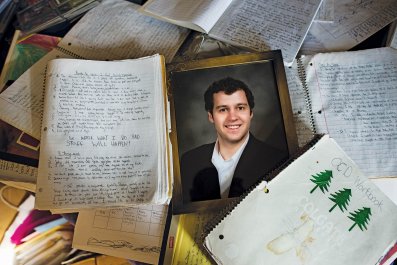
"You know you could have twins," the doctor warned her before the procedure. Decrette says she "freaked out…I just wanted one more baby." But because it seemed like her best chance at another child, she decided to do it anyway. Her twin preemies were born two months early, underweight at 3.5 pounds each, after a difficult pregnancy requiring an unusually high amount of time on bed rest.
Despite their premature birth, her twin daughters are now "perfect," she says. "It's such a blessing to have them." But looking back, Decrette, now 49, believes, "the best thing would be one embryo, one baby."
That was 10 years ago. Today, fertility doctors would almost certainly have pushed her away from the idea of a two-embryo implant; with new techniques that make single-embryo transfers much more likely to work, the potential hazards that come with multiples are, they say, simply not worth it.
Twins and triplets come with short- and long-term health risks to both mother and baby. IVF twins are more likely to be born earlier than singletons: There is a sevenfold risk for delivery before 32 weeks, according to a 2004 Danish study published in Acta Obstetricia et Gynecologica Scandinavica. The stillbirth rate is doubled in twins compared with singletons, and mothers of twins have a 4.6 times higher risk for cesarean section, a surgery most mothers hope to avoid because of the risks, longer recovery time and possible harmful effects on the babies. Twins are also nearly twice as likely to be admitted to a neonatal intensive care unit.
The risk of multiples has long been an unfortunate cost of IVF. Since the first test-tube baby in 1978, doctors have been transferring multiple embryos to a mother's uterus in hopes of achieving one healthy fetus. Back then, doctors had no way of knowing which embryo would be the one, so "people were hedging their bets," says Dr. Robert Stillman, medical director emeritus at Shady Grove Fertility Center, the largest fertility program in the country.
But thanks to improvements in technology, fertility doctors today are much better at selecting healthy embryos to transfer. Most clinics can culture an embryo up to five days, instead of the two- to three-day limit in the past. This advancement, many believe, helps weed out abnormal embryos. Some clinics biopsy the embryos to find the chromosomally normal ones. This is key, particularly for hopeful older mothers: only 2 in 5 of a young woman's eggs are chromosomally normal, and that figure decreases with age. Time-lapse videos and other noninvasive analysis of embryos also offer some promise in helping doctors select and implant a single embryo with a high chance of success.
According to the American Society for Reproductive Medicine (ASRM), in 1978 the pregnancy rate for IVF was only 0.4 percent. By 1997, that number had risen to 25 percent, and by 2013, with all the new technologies in place, it hit 65 percent. Meanwhile, studies have shown that transferring one embryo in two consecutive cycles produces the same pregnancy rate as a double-embryo transfer—without the risk of twins. In other words, "we no longer need to hedge our bets," said Stillman.

That's why the latest industry guidelines, published by the ASRM in 2012, advocate elective single-embryo transfer (eSET), especially in younger women with healthy embryos and no previous IVF failures. "The optimal outcome of an IVF cycle," the ASRM report says, "is the birth of a healthy singleton."
"How many parents would make a conscious decision that would cause health risks for their kids?" asks Dr. Richard T. Scott Jr., founding partner of Reproductive Medicine Associates of New Jersey and a professor of reproductive endocrinology at Rutgers University's Robert Wood Johnson Medical School. If single-embryo transfer was the standard of care, it would "allow people who want to have kids to have them safely—one at a time," he says.
The problem, though, is that despite the industry guidelines and the clear risks of multiples, doctors and patients in the U.S. have been slow to adopt eSET. In fact, last year only 12 percent of all IVF procedures in the U.S. were eSET. Many women are hesitant to do one embryo transfer at a time because of the cost savings in transferring more than one embryo at a time. For example, at the HRC Fertility clinic in Encino, California, one IVF cycle costs $7,400—below the national average of $12,400—but an additional frozen embryo transfer would cost $3,500. Which means if you put in one embryo at a time, each time would cost an additional $3,500. And many insurance plans limit the number of cycles they'll cover—if they cover IVF at all.
"The problem with in vitro is that most of us are paying out of pocket for it, so when the doctor suggests you transfer only one embryo at a time, it sounds ridiculous," says Phoebe Kannisto, who, while trying to have a fourth child, suffered from infertility and decided to start IVF. "You're giving me one shot at pregnancy? That's insane." She ended up having three embryos transferred at once—and had triplets.
To convince parents to go with eSET, some clinics are offering financial incentives. Shady Grove offers women half off the next embryo transfer ($5,600) if they put in only one. It also offers a shared-risk program, which allows qualifying patients to pay in advance for six cycles. The baby is guaranteed by cycle No. 6, or your money back. This encourages patients not to transfer more than one embryo, since they are not paying for additional cycles.
At least one major insurer is also getting on board. Aetna, which provides medical insurance to approximately 23.6 million Americans, now offers a financial carrot for patients who choose eSET: If the first IVF cycle fails, Aetna will cover the costs of the second transfer. "We're hoping that this will be the wave of the future," Stillman said. "It's in insurance companies' best interest: IVF costs are minimal. Premature twins or triplets can present lifelong complications and costs."
Still, a small set of professionals disagrees with the ASRM recommendations. "I'm against eSET as a standard procedure," says Dr. Norbert Gleicher, the founder and director of the Center for Human Reproduction IVF clinic and the president of the Foundation for Reproductive Medicine, a New York-based nonprofit. Gleicher says the studies comparing twin births to singletons are flawed: A statistically correct analysis would be to compare a twin pregnancy to two consecutive pregnancies, he argues in a 2008 article published in the journal Fertility and Sterility. In those cases, "all significant risks disappear," says Gleicher. And with no health risk, "the issue is really not whether eSET is good or bad. The issue really starts with the question, Are twins a bad outcome or a good outcome?"
For many in the medical profession, multiples are such an unfavorable outcome that they advise "selective reduction," the medical procedure of terminating a multiple. Selective reduction is common for triplets and beyond, but also presents risks to the other fetuses—not to mention a moral dilemma for expecting parents.
Marie, a 34-year-old teacher, was terrified of having a high-risk pregnancy of multiples, and she already had a 5-year-old son from IVF with her girlfriend. But when IVF wasn't working—they'd put in one embryo at a time, twice—her doctor did a double-embryo transfer. When Marie saw two heartbeats on the ultrasound, "I was devastated," she says, because she didn't want to have a reduction. But by the next ultrasound, the twin vanished. "I was incredibly relieved," she says. Her son is now 10 months old. "Now we're done," she says. "I'm definitely not doing this again."
But for other patients, twins are a risk they are willing to take. Bonnie Levine started IVF at age 42, and time was of the essence. "At my age," she says she thought at the time, "my eggs are declining." She went to a clinic geared toward older women—one, she found out, that actively promotes single-embryo transfers. She fought back. "They pretty much wanted to transfer one embryo every time, but whenever I could, I insisted on two, even three," she says. "I'd already gone through a lot of fertility treatments, and although I preferred one child, I was open to having twins."
What really drove her decision was the emotional cost of single-embryo transfers. "When you do a double-embryo transfer, it hastens the process. It only takes one month instead of two, one two-week wait to find out if you're pregnant, one disappointment if you don't," she says.
Now 44, she is still not pregnant and looking into other option, such as donor eggs and adoption. "This whole process takes so much out of you."