In one of the last photographs my family took of my grandmother, she looks as if she's been in a fistfight. Jean Bass Tinsley is lying in a hospital bed in Athens, Georgia, wearing a turquoise button-up shirt and staring blankly at the camera. A bandage obscures her fractured skull, along with the bridge of her bloodied nose. She is 91 years old.
My grandmother essentially did this to herself. In June 2013, she fell out of her wheelchair headfirst, after ignoring her caregivers' warnings not to get out of bed without help. Earlier that year, she'd broken both of her hips, in separate falls. Before that, her pelvis—all while trying to do what for most of her life she'd managed just fine on her own: walk.
In her last year, dementia crept into my grandmother's mind. The staff at her long-term-care facility plotted ways to protect her from herself. It's against the law in Georgia to restrain patients in such facilities, so they lowered her bed to the floor and put a pad down next to it. They even installed an alarm that went off if she left her mattress. My grandmother disabled the alarm, moved the pad and freed herself, repeatedly. In the end, she was both too weak and too strong.
Four months before Grandma died, my mother moved to Georgia to be with her. To prevent her from getting out of bed, nurses at my grandmother's facility began medicating her so heavily that she barely seemed alive. My mom insisted they stop drugging her, at which point Grandma's resolve (and penchant for injury) returned. Several times a week, Mom would call me, bawling, with the latest in my grandmother's saga. At one point, Grandma told my Aunt Cindy that she didn't want to "do this" anymore. That she was ready to die.
From across the country, I listened to these stories and wondered aloud if perhaps my grandmother had lived too long. Doctor-assisted suicide is illegal in Georgia, and even in my home state of Oregon, no physician would have helped her; she was no longer consistently lucid. My point was moot, but Grandma clearly wasn't going to recover. All that was left of her life was pain, confusion and suffering.

Give Me Liberty, Give Me Death
Last month, while traveling through Europe, I met a 65-year-old woman in Amsterdam determined never to wind up like my grandmother. Jannie Willemsen is in near-perfect health, but as we sat down at a small café, she showed me papers that laid out the circumstances under which she no longer wants to live: if she's severely and permanently lame; if she can no longer leave the house on her own; if she's dependent on others to eat, drink, shower and put on her clothes; if she goes blind or deaf or is suffering from dementia—most of what my grandmother experienced in her final months. "I'm an autonomous person," Willemsen says. "For me, it seems a disaster not to be able to go out and visit friends, to a concert, to the theater."
A kind and lively woman, Willemsen is now retired from her career as a biologist. She and her husband signed their power of attorney papers in 1997, just after doctors diagnosed him with intestinal cancer. Neither had any interest in living longer than what felt natural; they wanted to decide for themselves when they would go. Willemsen's husband died in 2004, not from cancer but a heart problem. He was "lucky," she says, because he didn't suffer for long. After his second operation to remove intestinal tumors, his heart stopped. Willemsen had to produce his papers, she says, to convince the doctors not to resuscitate him. "They said, 'Our first concern is keeping him alive,'" she recalls. But that's not what he wanted. It's not what she wants, either.
What she wants, if the circumstances merit it, is doctor-assisted euthanasia, which is booming in the Netherlands. In 2013, according to the latest data, 4,829 people across the country chose to have a doctor end their lives. That's one in every 28 deaths in the Netherlands, and triple the number of people who died this way in 2002. The Dutch don't require proof of a terminal illness to allow doctors to "help" patients die. Here, people can choose euthanasia if they can convince two physicians they endure "unbearable" suffering, a definition that expands each year. Residents here can now choose euthanasia if they're tired of living with Lou Gehrig's disease, multiple sclerosis, depression or loneliness. The Dutch can now choose death if they're tired of living.
That act is technically illegal in the Netherlands. Those who aid in euthanasia can face up to four and a half years in prison. But since the early 1970s, the Dutch government has treated assisted suicide much the same way it handles cannabis users: by looking the other way, honoring the public's overwhelming view that people in the Netherlands should have the right to die. Since 2002, euthanasia has officially been decriminalized here, so long as certain criteria are met.
Other countries are now edging closer to the Dutch model. On February 6, the Supreme Court of Canada struck down a ban on physician-assisted suicide, joining Luxembourg, Belgium and Switzerland on the list of Western countries where euthanasia is fully legal. Switzerland has allowed assisted suicide since 1942, so long as patients "participate" in the administration of life-ending drugs (by ingesting them). The law doesn't require that a patient be a Swiss national, which has encouraged "suicide tourists" from other countries to book one-way tickets there.
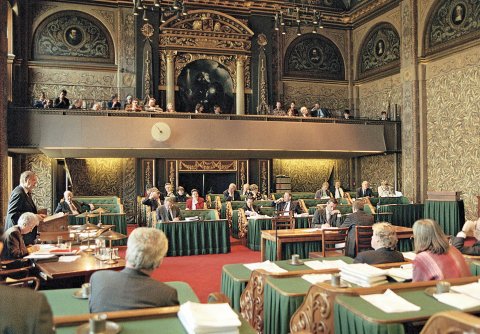
In France, lawmakers are debating a bill that would give doctors the right to place patients into a deep, painless and permanent sleep. In the U.K., legislators are now considering an "assisted dying bill" that would legalize euthanasia for the first time. "I think in 10 or 15 years, a lot of Western European countries are going to have a law, one way or another," says Fione Zonneveld, communications director for Right to Die-Netherlands, an Amsterdam-based organization that lobbies for the expansion of euthanasia laws. "It's a snowball."

Assisted suicide has long been taboo in the U.S., thanks in large part to Jack Kevorkian, the Michigan euthanasia activist who claimed to have assisted in the suicides of at least 130 people. Today, more than 15 years after Kevorkian's conviction on charges of second-degree murder, Americans are taking a second look. Assisted suicide is legal in Oregon, Washington and Vermont; in New Mexico and Montana, doctors are permitted to prescribe medication to end patients' lives. Last year, a 29-year-old California woman with terminal brain cancer moved to Oregon so she could legally end her life. A newlywed, Brittany Maynard wrote articles and appeared on television to discuss her decision. Some lauded her as brave; others condemned what they called her cowardice. Since Maynard died on November 1, lawmakers in six states have proposed right-to-die laws, and politicians have promised to do so in eight others. A Gallup poll conducted last May showed that nearly seven in 10 Americans believe physicians should be able to "legally end a patient's life by some painless means." The figure has bounced between 65 and 75 percent since 1996, after a steady climb from 36 percent in 1950.
The march toward euthanasia mirrors a trend spanning continents today: a growing number of countries are placing more value on individual freedom. This worries religious leaders, ethicists and disability advocates. Assisted suicide may ease suffering, they say, but it threatens our most vulnerable citizens—the elderly and the disabled, who already struggle to justify their lives. "I like autonomy very much," says Theo Boer, a professor of ethics at the Theological University Kampen in the Netherlands. "But it seems to have overruled other values, like solidarity, patience, making the best of things. The risk now is that people no longer search for a way to endure their suffering. Killing yourself is the end of autonomy."

The Wrong Way to Die
Last year, within the span of a few weeks, both of my parents sent me a story in The Atlantic by American oncologist Ezekiel Emanuel. The headline was "Why I Hope to Die at 75." My mother added in a note: "I think 80 is my number."
It wasn't the first time my parents dropped a morbid little bomb on me. In 2011, my mom emailed me with the subject line "I want to go on record," and the body read, "If I die at the hand of another, I don't want anyone taking a life to avenge my death." My dad used to tell me he wanted to be pushed out on an ice block when it was time for him to go. (I get it, OK? You guys are both going to die someday. Can I go back to watching Breaking Bad now?) They want to be sure I understand that they won't cling to life when there's nothing in it worth clinging to.
On suicide, however, they disagree. My father is convinced he'll find a way to die peacefully, even if by his own hand. "I'll take some aspirin, drink some fine whiskey and it'll be done," he told me recently. My mother insists she will never commit suicide. Her father shot himself in the head when she was 29 so he wouldn't have to undergo surgery to repair a ruptured vein in his esophagus. "It's a selfish act," she told me between tears. "It denies your loved ones the ability to be with you and take care of you."
Around the world, there are many who don't see it that way, and they've found plenty of like-minded physicians to guide them toward death. But it's not exactly a comfortable practice. Most doctors find euthanasia counterintuitive to the Hippocratic oath and terrifying. It's irreversible.
For Bert Keizer, that fear has subsided with time. He's a Dutch physician who has, in 33 years of practicing medicine, assisted the deaths of dozens of patients—mostly without regret. His first few cases were difficult, he told me in a phone interview, because they made him afraid. Not of prosecution but because of the finality of the act. "The fear is of doing something to a person you know can never be rescinded," Keizer says. "I never had an easy [death]." But over time, he says, that angst subsided. Keizer has grown increasingly at ease with injecting patients with a lethal dose of sodium thiopental and then a muscle relaxant, knowing he is bringing suffering to an end.

When Keizer agrees to help someone, he says it's usually obvious it's the right thing to do. The last patient he euthanized was an American expatriate who had lived in the Netherlands for 15 years. The man was 78 and had suffered a cerebral hemorrhage; he was unable to walk and barely able to speak. His wife had died a year earlier, which is why the first time the man asked Keizer for help, the doctor refused. "You have to come to terms with the fact you're mourning your wife," he told his patient. Eight months later, the man changed Keizer's mind. He could no longer wash himself, was incontinent and his condition was unlikely to improve. In summer 2013, Keizer agreed to help the man die. He's confident that was the right thing to do.
It's common for a physician to say no to a first request, Keizer says, in part because people sometimes change their minds. "I know we planned on it just before Christmas, but I'd like to hang on until February," he's had patients tell him. "If someone says that, as a doctor, you think, Oh my God, what am I doing? And I have to say, 'Look, I'm sorry, but this is the end of the line for me. I'm no longer willing to talk to you about euthanasia.'"
Every doctor who assists a suicide is likely to have at least one case he wishes he could take back. For Keizer, it was a 55-year-old man with lung cancer. The man had already undergone chemotherapy and radiation; oncologists "put him through the paces," Keizer says, "and at the end of the line he was still going to die. He was furious with his doctors, that they had led him astray all these years." When the man asked for Keizer's help 25 years ago, it was out of "an anger against life. I helped him, supplied him with an overdose, but years later I realized it wasn't right. It was a revengeful act. He died not with a smile on his face but with this bitter expression. That's not the way you should die."

Death Is Contagious
In the Netherlands, there are hundreds of people dying for reasons never anticipated when the law was passed. To understand why, I went to see Zonneveld at Right to Die-Netherlands. Her organization also helps members draft living wills and power of attorney papers, like the ones Willemsen showed me. Taped to the dry erase board in her newly refurbished office is a Dutch comic strip. "I consider my life completed, and want to die," a patient says. A doctor responds "OK" and produces a pistol. "Oh, no, I meant a soft death," the patient says. "Ah," the doctor says, and attaches a silencer to the gun.
Beneath that comic is a chart that shows a huge spike in the group's membership, from about 120,000 in 2010 to 160,000 today. On average, between 30 and 50 Dutch citizens sign up daily. Members pay 17 euros a year in exchange for end-of-life counseling and help with their documents. Last year, Right to Die-Netherlands used its funding surplus to open a mobile clinic. Twenty-three nurse-doctor teams now stand ready to be dispatched to people's homes—to dispatch those people.
In the first few years after the Netherlands decriminalized euthanasia in 2002, the number of cases declined. Then, in 2007, the statistics began a steady climb, an average jump of 15 percent a year. Keizer admits he "didn't see it [this growth] coming." The situation has put him and other doctors in the country in an ethical quandary. "It's a feeling of not being quite certain about where you're going," he says, though he adds, "We're talking about 5,000 people out of 140,000. That's not an epidemic."
He figures Dutch autonomy has the most to do with the steady increase in assisted suicide. More than 90 percent of Dutch citizens polled say they support the law, though only 20 percent say they would choose to die that way. But euthanasia has in some form been passively allowed here for decades. There had to be other reasons for the surge.
Boer, the ethicist, has some theories. Once a supporter of euthanasia, he's now one of its most vocal critics. Among the reasons for the euthanasia boom, Boer suggests, is propaganda. Over the past decade, he says, Dutch journalist Gerbert van Loenen has been tracking a series of documentary films that depict euthanasia in a wholly positive light. "They do ask certain questions," Boer says. "But they systematically ignore most critical questions, so that the general public is presented with an opinion that is completely good, and has no risks. This is contagious."
Another key factor: It's getting easier each year to qualify for euthanasia. In the beginning, most of those eligible were terminally ill. Now doctors are helping people die if they no longer want to bear depression, autism, blindness or even being dependent on the care of others. "There are increasing numbers of double euthanasia—one of the partners is terminal and the other partner is care-dependent, they don't want to live alone," says Boer. One in 10 of the past 500 dossiers he has read contains some reference to "loneliness," he adds. "Those are the cases where I have become increasingly uneasy."
The numbers support Boer. In 2012, 13 patients were euthanized after convincing a doctor they were suffering unbearably from mental illnesses ranging from depression to schizophrenia. The following year, the figure more than tripled, to 44. The number of patients with dementia who killed themselves grew from 43 in 2012 to 97 in 2013. "I'm afraid," Boer says, "the situation in the Netherlands is out of control."
In 2005, lawmakers decriminalized another form of euthanasia—for babies. In recent years, the number of cases of newborn euthanasia has declined—because parents are acting sooner. The country introduced a new system of prenatal screening that allows parents to terminate pregnancy if ultrasound results reveal severe congenital malformations within 20 weeks of conception.

The Dutch didn't stop at babies. Minors in the Netherlands are now allowed to choose euthanasia, too. Children ages 12 to 15 may ask to die if they can get parents' permission. After age 16, young people can make the decision with only "parental involvement."
Pediatrician Eduard Verhagen helped establish the Dutch euthanasia guidelines for infants. He says the law should go further. "If we say the cutoff line is age 12, there might be children of 11 years and nine months who are very well capable of determining their own fate and making their own decisions, but they're not allowed to ask for euthanasia."
It is hard to imagine an American pediatrician making that argument. But no one envisioned euthanasia in the Netherlands would expand the way it has in the past 13 years. Perhaps the U.S. isn't far behind.
Doubts and Double Suicides
The euthanasia debate is often reduced to horrifying anecdotes. A doctor in Switzerland is under investigation for helping French twins with schizophrenia kill themselves. In Belgium, where assisted suicide cases rose in 2013 by 27 percent to 1,816, a Brussels man arranged the "double euthanasia" of his parents so they no longer had to be alone. My grandmother's last days, on the other hand, are seemingly easy fodder for assisted suicide supporters. The reason France is discussing euthanasia is partly because of two cases from 2013: both double suicides, both couples in their 80s. One of the couples ended their lives in a luxury hotel in Paris, ordering room service and then asphyxiating themselves by putting plastic bags over their heads. Hotel staff discovered them holding hands, with a note next to them that claimed "the right to die with dignity." The other couple died in a hospital: The 84-year-old man shot his terminally ill wife in her bed, then turned the gun on himself.
But it's dangerous, euthanasia opponents say, to view the issue solely from the perspective of a few individuals determined to end their lives. There are great risks associated with allowing doctors to help people check out early, they say. Paramount among them, says Wesley J. Smith, a California lawyer and consultant for the International Task Force on Euthanasia and Assisted Suicide, is that people have forgotten the meaning of suffering. "There is a new view of suffering, that it's the worst of all possible experiences," Smith told me in a phone interview, "and that the role of society is to prevent it, as opposed to mitigating it."
Financial considerations could also creep into discussions that should never involve money. In the Netherlands, as in many developed countries, the number of elderly citizens is expected to increase by 30 to 40 percent in the coming two decades. Euthanasia, critics say, adds a dangerous option in this context: a way for societies to nudge the elderly to quicker deaths.
In the U.S., euthanasia opponents contend the profit-driven health care system and its slow takeover by cost-cutting managed-care companies pose major ethical risks. "There's a lot of pressure in the system already," says Diane Coleman, the president and CEO of Not Dead Yet, a disability rights group that lobbies against the legalization of assisted suicide and euthanasia. "We see people denied the care they need for economic reasons. Assisted suicide is the cheapest kind of treatment that could be offered by the system. These pressures are a reason for concern."

In 2008, Oregon Medicaid officials sent a letter to Barbara Wagner and Randy Stroup after the couple sought treatment for her lung cancer and his prostate cancer. The state denied their (costly) treatment, but on a list of alternative options, it offered to pay for assisted suicide. The couple went public and the state changed its mind, but Smith contends that the more we embrace euthanasia, the more government officials will back away from paying to treat its weakest members.
Accountability is a huge problem with assisted suicide, critics say. In the Netherlands, a doctor must report the cause of such deaths to the coroner. The case is then reviewed by one of five regional Euthanasia Committees, consisting of a doctor, a lawyer and an ethicist. But that review happens after the patient is dead, and it's only to determine whether a doctor might be charged with a crime. The review committees have deemed about five cases per year to be illegal since 2002, but no physicians have been prosecuted. "The doctors always promised not to make the same mistake again," Boer says.
In light of the Dutch experiment, critics say there is no way to legalize assisted suicide without accepting the risk that vulnerable people will be pushed to their deaths—by the health care system, by their own guilt or by abusive family members or caregivers. "We don't think any set of safeguards is sufficient," Coleman says. "We need to respond to the desire to die with the message, 'No, how can we help you? How can we be with you?' That's the real compassion people deserve."
As the euthanasia movement grows, critics in America and beyond are calling for a better approach to the way we end our lives. In November, the surgeon and writer Atul Gawande published Being Mortal, a groundbreaking book that argues for wholesale change in the philosophy of health care, a departure from the American fixation on survival to a focus instead on enabling "well-being."
As for euthanasia, Gawande is torn. He acknowledges that people "want to end their stories on their own terms," and that "we inflict deep gouges at the end of people's lives and then stand oblivious to the harm done." He also points out that American doctors rightly allow people to refuse food, water, medication and treatments (and therefore end their lives). But the Dutch model is "a measure of failure," he writes, because it forgets that the ultimate goal should be "not a good death but a good life to the very end. The Dutch have been slower than others to develop palliative care programs that might provide for it. One reason, perhaps, is that their system of assisted death may have reinforced beliefs that reducing suffering and improving lives through other means is not feasible when one becomes debilitated or seriously ill."
Instead of suicide assistance, Coleman argues, doctors should offer better suicide prevention. When asked why they want to end their lives, people invariably check the same boxes: They've lost autonomy, or don't want to be a burden on friends and family. But allowing physicians to help patients commit suicide is a cheap out, she says. What they should do instead is to help people make their lives livable, even if that's just for the last few weeks.
"The majority of Jack Kevorkian's victims were people with disabilities who were not terminal," Coleman says. "I saw him on TV once say, 'Well, they need it more, because they're going to suffer long.'"
Coleman has herself confronted this so-called need. After a lifelong battle with congenital myopathy, a neuromuscular disorder, she was hospitalized in 2012 with acute respiratory failure after a bout with viral pneumonia. On her way to the hospital, one of the EMTs asked her husband if she had a do-not-resuscitate order. "Something about the way they asked the question led him to not only say 'No' but also to explain to them that I have a full-time job," she wrote later. "He felt that this changed their tone." A month later, Coleman was again hospitalized with chest congestion, and one of her doctors questioned whether she wanted it treated. "He looked at me in my wheelchair with what I'm sure he viewed as sympathy for my condition and a genuine concern to be sure that he knew what I wanted. But I also felt sure that he wouldn't have spoken that way to a nondisabled woman at age 58." Again, Coleman said, "I have a full-time job," and "he backed off, stopped talking and left."
Who's Ready to Die?
The day we met, Jannie Willemsen was on her way to visit an old friend who lives about 40 miles outside of Amsterdam. Each of these gatherings may as well be the first, she tells me. Willemsen's friend is 87 and suffering from dementia. She remembers nothing of their past encounters, nothing of their four decades of friendship, not even Willemsen's name. "It's so nice that you come to visit me," her friend said when she got there, as she ate in the restaurant of her nursing home and nibbled on chocolates. "She's still very kind. But she doesn't recognize me."
Willemsen dutifully visits anyway, but less often now. If she derives something from these encounters, it's a reminder that she is determined never to be swallowed by such a haze, never to spend even a day bumbling around a nursing home. "I'm happy there is an end of life," she says. "Some people believe God has given us life, and that he should be the one to take it. I think when you get older and older, there comes a time when you don't feel at home in this world, where you don't understand it any longer, where you can't explain it."
My grandma reached that point, but it's not how I remember her. Once, on a sticky summer day in 1998, I surprised her, sneaking over to her century-old Craftsman house in Calhoun, Georgia. I was 21 and hadn't seen her in a decade. How funny would it be, I thought, for me to walk up her driveway unannounced? I was halfway through my first internship at a small newspaper in Alabama, only a few hours' drive to her place, so one Saturday I printed out a set of MapQuest directions, journeyed across the border, parked down the block and sauntered toward the screen door to the back porch, full of mirth and mischief, anticipating the stunned look on Grandma's face. Would she even recognize me? As I went to knock, she emerged, shot me half a glance and said, "I have to run to the store. I'll see you in a bit." She walked right past me, got in her car and drove off.
This is how I will always remember my grandmother, as a tough woman to rattle. I wasn't there when she died and didn't participate in the decisions my family had to make about her final days. It was easy for me to judge from afar that Grandma had lived too long. My mom didn't see it that way.

"It made me so angry at the time, when people suggested that she was ready to die and I should just give up on her," she recently told me. "Those last days were brutally hard, but rich with meaning. I taught her to knit again, to try and keep her busy and take her mind off the boredom and discomfort of being confined to a wheelchair. One afternoon we went through her old photo albums, and she told me about her high school days, remembering the names of people and events. It was amazing, and I'll never forget it."
My mother says she would never have chosen euthanasia; not for her mom, not for herself. But she had to make difficult decisions throughout my grandmother's final months. After Grandma stopped eating on her own, my mom and her siblings decided against feeding her intravenously, but they didn't reject fluids. "I'm not going to let my mom die of dehydration," she told a doctor.
Someday I may be faced with the same impossible choices about my own parents. Both recently turned 70.