The deadly outbreak of Ebola, the largest in recorded history, comes as little surprise to scientists. In the light of recent research, expect to see more global public health emergencies, faster spreading scourges and more novel diseases. True enough, modern technology has brought us a range of extraordinary tools, from diagnostics to drugs to global, instantaneous communications. But the relentless rise of modern civilisation has also made the possibility of a pandemic greater than at any time in history.
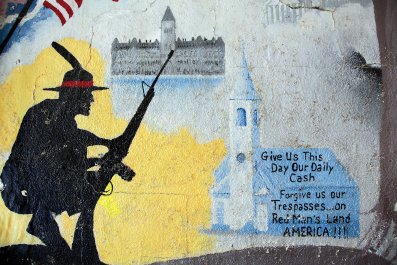
Emerging diseases that have devastating effects internationally, with millions infected and billions spent, are all foreseeable consequences of changes in the way we live our lives. This is not simply the price of our success in dominating the planet and its ecosystems but, importantly, of allowing so many of the planet's human inhabitants to live in poverty. The Ebola emergency reminds us that we now have the conditions for a perfect microbial storm.
Most human infectious diseases originated in animals and, as human populations and their road networks expand, as we clear more land for agriculture, hunt for wildlife and trade more animals, they are coming into contact with more animal diseases, explains Angela McLean of Oxford University's Institute for Emerging Infections. Meanwhile, we are increasingly farming vast numbers of domestic animals that can provide reservoirs for existing bugs and fertile breeding grounds for new ones. There are also unprecedented opportunities for rapid spread, thanks to air travel, as in the current Ebola outbreak.
The role of wild animals in the origin of novel diseases was laid bare in 2008 when Peter Daszak, now president of the EcoHealth Alliance, Kate Jones of the Institute of Zoology and University College London, and colleagues from Columbia University, New York, analysed 335 emerging diseases from 1940 to 2004. Maps which correlated disease with human population density, rainfall and wildlife biodiversity revealed that disease emergence events have roughly quadrupled over the past 50 years.
Some 60% of the diseases spread from animals to humans – such diseases are called zoonoses – and the majority of those came from wild creatures. The HIV/AIDS pandemic started from human contact with chimps and sooty mangabey monkeys; recent outbreaks of SARS (Severe acute respiratory syndrome) originated in Chinese bats; CJD (Creutzfeldt-Jakob disease) in cattle; and MERS (Middle East Respiratory Syndrome) to camels. The Zaïre subtype of the Ebola virus responsible for human outbreaks in Gabon and the Republic of the Congo was linked to the handling of the carcasses of great apes that in turn had been infected by fruit bats. The global map of emerging disease revealed the hotspots span sub-Saharan Africa, India and China, with smaller spots in Europe, and North and South America. They tend not to be in the richer countries in the North that can afford surveillance but in relatively impoverished areas such as the tropics, a region rich in wildlife species and under increasing human pressure, and in dense human populations, where one would expect them to take hold more easily.
The risks are now worse than suggested in their 2008 study, says co-author Marc Levy, deputy director of the Center for International Earth Science Information Network at Columbia University in New York. They had assumed populations would fall faster than they have. Moreover, political violence and instability has "led to refugee flows and deliberate incursions into wild areas where rebels find timber, wildlife and minerals to finance their activities. In the case of Ebola, we have also seen that it is difficult to deal with effectively when public trust in a government is low".
In 2010, another study also involving Jones and Daszak, showed that species losses in ecosystems spur rises in pathogens as we intrude into areas of high biodiversity. This is significant because current extinction rates are estimated at 100 to 1,000 times higher than in past epochs, and are projected to increase at least a thousand times more in the next 50 years.

Though more work must be done to understand the mechanisms, loss of biodiversity threatens human health in various ways. Wetland degradation may force migrating waterfowl that harbour avian influenzas into sites where they have contact with domestic fowl. Moreover, animals, plants and microbes most likely to disappear as biodiversity is lost can buffer infectious disease transmission: for example, opossums are able to effectively kill disease-carrying ticks but when opossum populations decline, tick populations can then flourish in the Virginia white-footed mouse, which can reproduce quickly along with both the blacklegged tick vector and the pathogen that causes Lyme disease.
Domesticated animals also play an important role. Influenza can infect pigs and birds as well as humans, for example. When it comes to developing countries, pig and poultry farming is intensifying more rapidly than other farm sectors. With more animals being raised in more concentrated spaces, so farmers and vets have a markedly increased risk of infection with flu viruses.
To turn into an epidemic, any microbe must not only be able to infect people but also spread efficiently. Overall, it needs at least one new victim for every old one who either dies or recovers and purges himself of the microbe. If the average number of new victims per old drops below one, then the disease fizzles out.
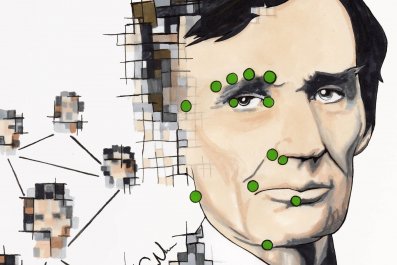
We now have a deeper understanding of the role of air travel in the spread of disease. Studies published at the end of last year by Dirk Brockmann, now at Humboldt University and the Robert Koch-Institute in Berlin, and Dirk Helbing at ETH Zurich, led to a new mathematical theory for understanding the spread of epidemics. This focuses on travel hubs and links so that if the flow of passengers from point A to point B is large, the effective distance is small and vice versa.
From the perspective of Frankfurt, other metropolitan areas such as London, New York or Tokyo are effectively no more distant than geographically close German cities such as Bremen, Leipzig or Kiel. With this new theory, scientists can track the origin of an outbreak with greater confidence, compute the speed of epidemic spread and forecast when it is likely to arrive at any location.
Meanwhile, the advance of medical science presents its own problems. This year saw accidents involving anthrax and the deadly H5N1 influenza virus, and the discovery of old vials of smallpox in a Food and Drug Administration laboratory in Maryland, US (before HIV, the smallpox variola virus was thought to be responsible for the loss of more human life than all other infectious agents combined). Biosafety experts fear that even highly secure facilities could place the public at risk.
Many are also uneasy about work to create highly pathogenic strains of disease – to understand, for example, why one flu strain is more deadly than another. One preoccupation is what made the 1918 H1N1 influenza virus, which killed 40 million people, so virulent. Another unease is about the potential use of genetic wizardry to use DNA sequences to recreate deadly pathogens, such as smallpox. "It's a trade-off between how much we learn and the risk," explains McLean. "I used not to worry about it. I do now."