In a simple home in the village of Mosebo, Ethiopia—an earthen floor and walls made of wood and mud—a woman sat on a mattress on the floor with her crying, 8-month-old son. The mother, Alemitu Kelkay, pressed him to her breast, and eventually he quieted down. A normal enough scene, for most. But when this boy, her third child, was born, he was underweight, weak and wouldn't breast-feed. Without proper care, he might have died.
That little boy is one of millions of babies born underweight annually, the vast majority in developing countries. The 15 million infants born preterm each year are susceptible to illness and likely to be underweight. (Not all underweight babies are preterm; Kelkay's son, for example, was full term.)
"Worldwide, preterm birth is now the leading cause of child death," says Dr. Joy Lawn, an epidemiologist at the London School of Hygiene & Tropical Medicine. "Direct complications of preterm babies kills more than 1 million children a year." A very preterm baby born in high-income countries has more than a 95 percent chance of living, but in the world's lowest-income countries, less than 10 percent survive.
Underweight and premature babies are usually put in incubators—devices that provide an enclosed, temperature-controlled environment for the newborn, keeping it warm so it can use its precious energy to grow. But the nearby health center where Kelkay gave birth, she told me, doesn't have them. As she spoke, chickens clucked in the background as rain began to drum on the metal roof. At one point, two large cows walked into the house and took shelter in one of the rooms. A calf followed and went into another room. The family, which grows crops like teff, barley and beans, shares the home with its livestock.
Luckily, Kelkay was provided with an innovative solution that can work anywhere, from the most pristine hospital halls in New York City to her modest home: kangaroo mother care (KMC), in which the mother acts as a living incubator by wrapping the infant directly to her chest. The skin-to-skin position keeps the baby warm and close to the breasts so it can feed easily, and it promotes bonding between mother and infant. The name comes from the model in nature: A newborn kangaroo lives in its mother's pouch, with easy access to her milk.
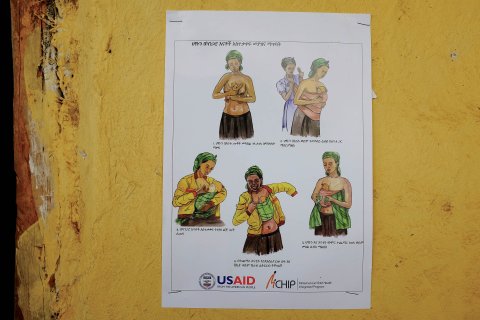
The technique was developed in 1979 by Edgar Rey, a doctor in Bogotá, Colombia, who confronted the challenges a neonatologist in a poorly funded clinic grapples with even today: not enough incubators and lots of infections. His solution did more than just cover for a lack of machinery. In Bogotá, infants would sometimes spend two to three months in incubators and were sometimes deserted by their mothers. KMC was a way to help mothers be more active in their baby's care and minimize the chances for abandonment. Skin-to-skin touch between mother and child has been shown in a small study to raise the mom's level of oxytocin, a hormone correlated with bonding behavior—and is also well known for helping breast milk flow.
KMC has been found to be so effective that some experts believe it should be used even when incubators are available. A 2010 study by Lawn estimated that KMC could save as many as 500,000 lives annually if practiced more widely. Lawn's study found that preterm babies cared for "skin to skin" had fewer complications than those in incubators. They also had better feeding and weight gain, stable temperatures and fewer infections. This last concern is one of the most serious. Based on her experience as a neonatologist in Africa, Lawn says that "usually we don't have enough incubators even in hospitals where we have them, and we put three or four babies per incubator. They infect each other."
KMC will never be the equal to a great neonatal intensive care unit (NICU) says Dr. Taraneh Shirazian, director of the global health program at Mount Sinai Hospital in New York City. For one thing, premature babies frequently have respiratory problems and might need oxygen or intubation, but "the reality in most places in the world is that there are no incubators and there is no NICU," she says.
Shirazian is the medical director of an organization called Saving Mothers, and she and a team of graduate students are developing a sling that they will eventually distribute for free in developing countries to help promote KMC. This is no BabyBjörn baby carrier meant to be worn over the clothes—the device keeps the baby right on the mother's bare chest.
In Ethiopia, KMC hasn't expanded as broadly as hoped, says Save the Children's Dr. Abeba Bekele, because it requires one-on-one training for nurses and mothers who are already too busy. Lawn says KMC is growing in popularity most quickly in the developed world—countries like Canada and Scandinavia. "People are redesigning neonatal intensive care units so that even babies who are being ventilated can be held skin to skin," she says. In fact, Shirazian's hospital, Mount Sinai, uses KMC to supplement the modern care it offers in the NICU. Reina Pearl, a nurse there, explains that when a preterm baby is stable enough, it will be taken from the incubator for up to an hour of KMC time with its mom.
"These things that it gives to the child, you can't give it any other way," Pearl says. The biggest reason is that it helps the mother boost her milk production—just 10 minutes of skin-to-skin time helps, she says. Plus, she adds, the NICU is stressful, and it is vital for parents to be involved in their child's care. "It's very hard to bond with a baby when they're in a box all the time."
Rob Verger traveled to Ethiopia with the International Reporting Project.