"The enemy of my enemy is my friend," as the old saying goes. When it comes to the global health crisis caused as modern medicine becomes powerless to fight superbugs, salvation could lie in harnessing their oldest enemy.
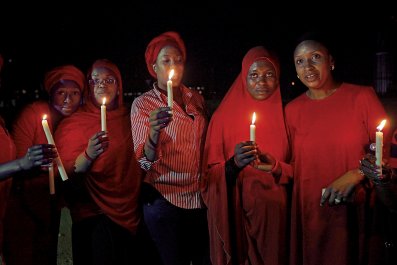
Every few days, half the bacteria on Earth are killed by the viruses that prey on them, known as phages, the most common organisms on the planet. Could we enlist their help? Today there is renewed interest in phages as warnings intensify that a "post-antibiotic" era looms, when a scratch could kill and major surgery is too risky to contemplate. Senior public-health officials talk of a "catastrophic threat," one comparable to that of climate change.
We've seen it coming. Alexander Fleming, who discovered penicillin in 1928, warned about the possibility when he accepted his Nobel prize in 1945. Resistance is inevitable, perhaps the most depressing implication of the evolutionary ideas of Charles Darwin. When treatment with an antibiotic begins, non-resistant bacteria are wiped out, leaving resistant cells to thrive. The overuse of antibiotics in agriculture – to promote livestock growth – and in hospitals drives the proliferation of drug-resistant bacteria.
A decade ago, most headlines focused on MRSA – the drug resistant strain of Staphylococcus aureus – and the superbug Clostridium difficile. Today, Klebsiella pneumoniae, a gut bug, has become resistant worldwide to the last line of antibiotics, the carbapenems. Gonorrhoea is also resistant to the last-resort antibiotics and resistance to antibacterials for urinary tract infections – fluoro-quinolones – is widespread.
The relentless rise of resistance, which causes people to be sick for longer as well as raising their risk of dying, has forced researchers to take a different approach. Enter the phage.
The first to identify them, in 1915, was English scientist Frederick Twort, though it was the French-Canadian Félix d'Herelle who first coined the term bacteriophages ("eaters of bacteria") and recognised their potential. He conducted the first human study in 1919, in which he gave a phage preparation to a 12-year-old boy with severe dysentery who recovered within days.
By the 1930s, phage therapies were being manufactured by companies in Europe and America. Soviet and German armies used them in the Second World War, but, with the rise of antibiotics in the West, phage therapy came to be regarded as suspect, though work continued in Eastern Europe, particularly the Tbilisi Bacteriophage Institute in Georgia.
Today, researchers are re-evaluating phages. Unlike traditional antibiotics, which can kill "friendly" bacteria, phages target particular strains, so one would expect them to be safer. By using a cocktail it is possible to sidestep potential resistance.
In August 2006 the US Food and Drug Administration approved spraying meat with a phage preparation created by the company Intralytix against Listeria monocytogenes. The following year, a promising trial was completed at the Royal National Throat, Nose and Ear Hospital, London, for Pseudomonas aeruginosa infections of the ear.
"I have seen an increasing research effort on phages that could be exploited therapeutically," says Dr Martha Clokie, of the University of Leicester. While other groups focus on MRSA, E. coli, Acinetobacter and Klebsiella, she is working with the AmpliPhi Biosciences Corporation on Clostridium difficile, which causes diarrhoea, vomiting and dehydration. In the US alone, 250,000 infections with this organism arise annually, resulting in 14,000 deaths and costing $1billion in excess medical costs.
Clokie has patented phages to combat Clostridium: "We have another six months of animal experiments and if they go as well as they are doing, we hope to move into clinical trials next year." A treatment could be ready in five years.
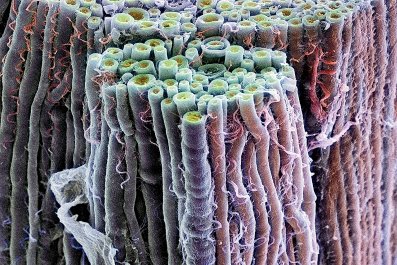
There is much we can learn from phages, even though they are nothing more than a scrap of genetic code in a protein overcoat. Measuring around 90 nanometres (billionths of a metre) wide and 200 nanometres long, the T4 phage looks like a moon lander, with "legs" that attach to an E. coli cell, and a tail to inject into the bacterium its genetic code, which carries instructions to build more. After making tens to hundreds of phages, the bacterium bursts, dies and spills newly-made phages to find more victims.
Instead of using whole phages, the bits that do the killing could be exploited. The ContraFect Corporation of Yonkers in New York, has used lysins, enzymes that digest ("lyse") the bacterial cell wall. One, called CF-301, combats MRSA. They are fundamentally different from antibiotics in that they kill bacteria on contact.
Another weapon was identified in phage T7, which targets E. coli, by a team led by Udi Qimron in Tel Aviv University, working with colleagues in America. They worked out the role of each of its 56 genes and found that one, called "0.4", impedes cell division. Block it, and the bacterium is prevented from multiplying. The 0.4 protein is much smaller than a phage so it should penetrate tissue better.
In the US, the Center for Phage Technology was set up in 2010 by Texas A&M University, the only state-funded centre dedicated to exploiting phage biology. The centre's director, Ryland Young III, said: "Our strategy is to work on -animal and plant applications because of the lower regulatory barrier. We have a cool system for -protecting grapevines against bacterial disease, as one example. If phages become obviously useful in these areas, eventually the public will demand changes in the regulatory system and allow use in humans without the draconian testing requirements currently in place for -chemical drugs."
To date, those that have been used in therapy have been isolated from the environment. The US biotech entrepreneur Craig Venter, who has achieved the remarkable feat of building a phage from scratch, is using DNA synthesis, bioinformatics and genome editing tools to create libraries of engineered therapeutic phages to fight superbugs. He says: "Perhaps in the future we'll be able to sequence an infectious agent from an individual patient to identify the target microbe and quickly design a custom phage therapy."
In the past, we have used and abused antibiotics derived from fungi and bacteria. Nevertheless, as long as we learn from our mistakes, phages could offer a potent weapon in the war against superbugs.